Drug-Resistant Superbugs: CIMAR Symposium Examines the Intersection of People, Animals, Food, and the Environment, and Their Impact on Health

Hover over slideshow to pause. |
April 9, 2019
The Tufts Center for Integrated Management of Antimicrobial Resistance (CIMAR) held its first symposium in Boston on March 18th. The event brought together over 175 clinicians and researchers from academia, medicine, and industry, all interested in fighting drug-resistant diseases via a “One Health” approach. One Health prioritizes the relationship among people, animals, the environment, and the foods we all consume as critical avenues by which drug-resistant bacteria spread from one to another
The Stuart B. Levy Tufts CIMAR Symposium was named to honor Dr. Levy, whose pioneering work in fighting antibiotic misuse and resistance was a key inspiration for CIMAR’s inception. Dr. Levy, who retired in 2018, had a decades-long career at Tufts University and Tufts Medical Center where he led the paradigm shift in how we view antibiotic stewardship, a term referring to the strategies healthcare professionals employ to ensure the judicious use of antimicrobial drugs. Dr. Levy’s work on mechanisms of antimicrobial resistance (commonly abbreviated as AMR) and spread of resistance determinants among microbes was among the first warnings of the dangers of antibiotic overuse in the emergence of drug resistance.
In 1981, Dr. Levy co-founded the Alliance for the Prudent Use of Antibiotics (APUA), a global research and advocacy organization with 66 chapters and members in more than 100 countries. His 1992 book, The Antibiotic Paradox: How Miracle Drugs Are Destroying the Miracle,proved prescient, and 20 years after its publication, the U.S. Food and Drug Administration issued guidelines for the judicious use of antimicrobial drugs in food-producing animals to minimize the emergence of AMR. Dr. Levy founded the Center for Adaptation Genetics and Drug Resistance at the Tufts University School of Medicine in 1992, and co-founded Paratek Pharmaceuticals in 1996, both in effort to advance AMR research and further the discovery of new drugs and combinations of drug therapies in the pursuit of saving lives.
Dr. Lonnie J. King, Vice Chair of the Presidential Advisory Council on Combating Antibiotic Resistant Bacteria (PACCARB), gave the Symposium’s keynote address. According to Dr. King, 60 percent of all human pathogens are zoonotic—or passed from animals to humans—including 75 percent of the emerging infectious diseases from the past three decades.
“Antibiotics have saved countless lives and are key to many medical treatments and procedures,” said Dr. King, who is also a Professor and Dean Emeritus of the College of Veterinary Medicine at Ohio State University. “However, over the past decade, antimicrobial resistance has become a crisis. The evolution of antibiotic resistance is now occurring at an alarming rate and is outpacing the development of new countermeasures capable of thwarting infections in humans. This situation threatens patient care, economic growth, public health, agriculture, economic security, and national security.”

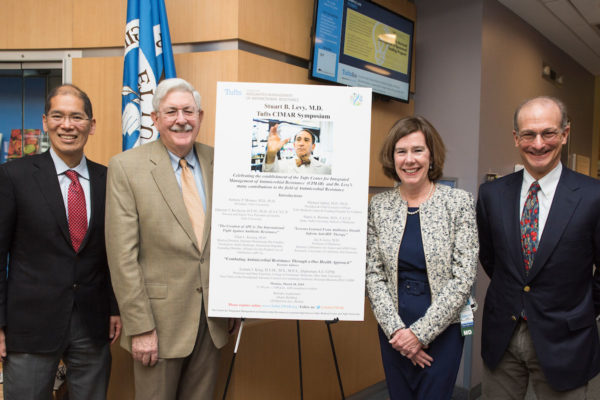
Keynote speaker Dr. Lonnie King, Professor and Dean Emeritus, College of Veterinary Medicine, Ohio State University, poses for a photo with the (L- R) Dr. John Leong*, Tufts U. School of Medicine Dean Harris Berman, Dr. David Snydman*, Dr. Helen Boucher**, Dr. Ralph Isberg**, and Dr. Deborah Kochevar, Tufts U. Provost ad Interim (* = CIMAR Leadership Team; ** = CIMAR Center Directors | Alonso Nichols/Tufts University)
Dr. King added that the interconnectedness of people, animals, the environment, and food has created an “unprecedented 21stcentury mixing bowl” that allows for the continual emergence and reemergence of diseases, including new drug-resistant pathogens. Despite these trends, he says, the scientific and medical response has remained largely reactive instead of proactive and confined to single areas of treatment instead of One Health.
“This is why I am so excited about CIMAR and what’s being done at Tufts to break [these trends],” he said. “We no longer have the luxury of looking at one domain by itself because then you’re only solving maybe one-third of the problem. If we don’t holistically look at an integrative strategy where we are looking at the domains of humans, animals, people, and our environment, I don’t think we are going to have the right strategies moving forward and we will have an incomplete answer to this very wicked problem.”
To highlight CIMAR’s commitment to combatting AMR through partnership and unique areas of expertise on both the research and clinical sides, the Symposium included introductory comments from Tufts University President Dr. Anthony P. Monaco as well as Tufts Medical Center President and CEO Dr. Michael Apkon.
“Tufts is committed to tackling important and complex problems,” said Dr. Monaco. “CIMAR draws on the diverse strengths of the University in this critical healthcare issue. It links basic science research with clinical expertise and patient outcomes.”
“We are profoundly grateful to Tufts Medical Center for their partnership in this new endeavor,” he added.
“All caregiving organizations have a social impact directly through care delivery,” said Dr. Apkon, “Academic centers like Tufts Medical Center have an amplifier or a turbocharger [in scholarship], which is taking what we learn from caring for tens of thousands and through research and educational programs, impacting the care of tens of millions.”
The Symposium’s scientific program included talks from eleven clinicians and scientists from across Tufts Medical Center and Tufts University’s three campuses in Boston, Medford, and Grafton, Mass. Each of these presenters is also part of CIMAR’s growing roster of core faculty. The core faculty come from a broad range of research backgrounds, but they have several things in common including their dedication to partnership and One Health, as well as their ability to straddle the multiple research areas at the core of the Center’s focus.
These areas include:
- Advocating for responsible antimicrobial usage (stewardship) in hospitals and other healthcare facilities, as well as for safer drug policies.
- Surveilling antimicrobial resistance among and between human and animal populations, as well as the environment.
- Educating young minds as early as high school in order to increase AMR awareness and cultivate a future generation capable of responding to the crisis.
- Developing combination drug therapies to treat AMR and slow the development of resistant strains in both human and veterinary medicine.
- Molecular mechanisms that control the development of drug resistance.
Dr. David Snydman, Chief of the Division of Geographic Medicine and Infectious Diseases at Tufts Medical Center (TMC) and a member of the CIMAR leadership team, is an advocate for stewardship and surveillance in healthcare settings. He described Clostridium difficile, a superbug that leads to more hospital-acquired infections than any other pathogen, as a marker of antibiotic overuse. Dr. Snydman and his team worked with six geographically dispersed medical centers on surveilling C. diff. The centers collected stool samples from patients who tested positive for C. diff infections and sent them to TMCfor analysis. The team observed increased resistance to the antimicrobial drug imipenem in particular. C. diff infections cost over $5 billion to treat annually, with approximately 450,000 cases reported per year and nearly 30,000 associated deaths nationwide.
Dr. Shira Doron, an attending physician at TMC, is also the hospital’s Physician Director of its Antimicrobial Stewardship program, which launched in 2003 to advocate for the appropriate use of antibiotics. The program has been a success in several ways, including that the hospital has seen a decline in antimicrobial resistance and in C. diffinfection rates. The program performs better than local and national benchmarks in antimicrobial usage, and as a result, TMC is the only hospital in the northeastern United States to have received the Infectious Diseases Society of America’s Center of Excellence designation. The antimicrobial stewardship group uses daily surveillance on an individual patient level and is working in collaboration with the Massachusetts Department of Public Health to bring these techniques into long-term care and nursing home settings.
Human care facilities aren’t the only places where stewardship matters. Dr. Annie Wayne from the Tufts University (TU) Cummings School of Veterinary Medicine described human-to-pet transmission of AMR microbes. She is collaborating with Dr. Doron and others from TMC and TU to study the feces of dogs and their human owners for signs of AMR after the dogs received outpatient treatments with antibiotics. Although the research is continuing, the team has found some evidence that humans can pass resistance genes to their dogs, resulting in the dogs becoming carriers of drug-resistant microbes. This, Dr. Wayne argues, is why all medical professionals dealing with the risk of resistance must take a One Health approach. Her group is working to implement antibiotic stewardship best practices from human medicine into veterinary hospitals.
Dr. Elena Naumova, Professor and Chair of the Division of the Nutrition Data Science at the TU Friedman School of Nutrition and Science Policy discussed efforts surrounding surveillance, tracking, and monitoring of AMR. To better control AMR in hospital settings, she proposed building a forecasting system to predict disease outbreaks. She added that building public data repositories would give researchers and clinicians worldwide the information they need to better understand the spread of resistance.

Researchers and clinicians presented 17 scientific posters at the Stuart B. Levy, MD Tufts CIMAR Symposium on March 18, 2019. (Alonso Nichols/Tufts University)
Scientists like Dr. Amy Pickering from TU’s Department of Civil & Environmental Engineering could benefit from such resources. Dr. Pickering studies AMR colonization in populations exposed to chlorinated and unchlorinated drinking water and human-to-animal transmission in developing countries. About one-third of the world has no access to clean water because of limited supply and sanitation infrastructure, and combined with unregulated drug usage, this leads to populations in low-income countries such as Bangladesh to have increased rates of AMR. In collaboration with the International Centre for Diarrhoeal Disease Research in Bangladesh, Dr. Pickering’s group focuses on disruption of AMR transmission by improving water quality. They performed a field trial in Dhaka, Bangladesh, looking at 100 drinking points where they installed chlorine “dosers,” which are cost-effective and do not require electricity to function. Their findings will show if children drinking safe water have lower rates of AMR colonization in their guts.
Vibrio choleraeis a multidrug-resistant pathogen most often found in the water supplies of Bangladesh and other lower-income countries. The bacterium causes cholera, a sometimes-fatal infection of the small intestine, and can spread rapidly in households and among communities. Dr. Andrew Camilli from TU’s Department of Molecular Biology and Microbiology has, along with his group and international collaborators, found three bacteriophages (or viruses that can invade and kill bacteria) that can prevent cholera from taking hold in the small intestine. They have discovered that when used together in a cocktail that is delivered orally, the bacteriophages significantly reduce infection and symptoms in animal models of cholera, thereby circumventing the problem of multidrug-resistance. Once funds are secured, Dr. Camilli and his team will begin clinical trials of the cocktail in humans in households in Bangladesh.
In addition to C. diff, patients in clinical care can be exposed toAcinetobacter baumannii, a multidrug resistant pathogen that has become increasingly difficult to treat as it has evolved resistance to most commonly used antibiotics. Dr. Ralph Isberg from TU’s Department of Molecular Biology and Microbiology and his lab are working to develop new strategies for eliminating strains for A. baumanniiresistant to the antibiotic fluoroquinolone. They find that fluoroquinolone-resistant strains have points of vulnerability that can be exploited by other drugs, therefore highlighting how combination or cocktail drug therapies could help curb AMR. Dr. Isberg is Co-Director of CIMAR along with TMC’s Dr. Helen Boucher.
TMC attending physician Dr. Roberto Viau Colindres discussed his work tracing AMR in Cambodia, particularly E. coli in meat and fish, which can result in human infections. His team found high incidences of the bug that were resistant to several antibiotics, but learned also that the whole E. coli bacterium does not need to be present for the transmission of AMR to occur. They hypothesize that even fragments of DNA from an animal-hosted bacterium can lead to infections in humans. Dr. Viau Colindres said that without CIMAR, this ongoing research project would not exist. Dr. Maya Nadimpalli, a postdoctoral fellow in Dr. Pickering’s lab at TU, has herself studied animal-to-human transmission of multidrug-resistant bacteria in Cambodia for several years. Following the 2018 CIMAR workshop, she approached Dr. Viau Colindres with the proposal to collaborate on this project.
There are several types of drug-resistant bacteria that can impact human health. Aside from the hospital-acquired, zoonotic, and food- and water-borne infections already discussed, sexually transmitted infections can also become resistant to antimicrobial treatments. In fact, according to the World Health organization, drug resistance in sexually transmitted bacteria is on the rise worldwide. Dr. Caroline Genco, Arthur E Spiller Professor & Chair of Immunology at TU’s School of Medicine, studies gonorrhea infections, of which there are over 100 million cases globally each year. Dr. Genco studies gonorrhea in China, which is part of the region where a third of these infections are found. Her project focuses on infected men with multiple sexual partners and their wives or other female partners who self-report as monogamous. Dr. Genco’s team isolated specimens and bacterial samples from the subjects and looked at their antimicrobial resistance levels among other factors. Dr. Genco noted that infected males tend to present with more symptoms than female patients, who might not have any symptoms at all. The team found that expression of AMR genes were four times higher in men than women. One hypothesis for this is that many of the men had taken antibiotics within 30 days leading up to the study, which killed the drug-susceptible bacteria, whereas all of the women in the study were asymptomatic and not taking antibiotics. Dr. Genco and her team are also looking into other possibilities including the fundamental differences in the sites of infection in men and women. The goal is to find treatments and treatment methods that will eventually curb resistant gonorrhea.
Researchers working on combination drug therapies can run into challenges in part because not all treatments work effectively when used together. In fact, some drugs that are effective on their own can actually harm patients when used in cocktails. Further, traditional laboratory testing for these synergistic versus antagonistic effects becomes exponentially difficult with the addition of each drug. Dr. Bree Aldridge from TU’s Schools of Medicine and Engineering studies Mycobacterium tuberculosis, the bacterium that causes tuberculosis. Tuberculosis is always treated with multidrug therapy over the course of at least six months. Dr. Aldridge and her lab have developed a new method called DiaMOND (Diagonal Measurement Of N-way Drug interactions) to rapidly measure how drugs act in combination. DiaMOND doesn’t require an exhaustive analysis of all drug behaviors in all possible dose combinations, which is what traditional testing entails. Instead, it targets only the most information-rich drug-dose combinations to predict combinations will be synergistic. This methodology is more efficient and less expensive than traditional testing, and it provides a framework for testing drug therapies for many diseases—not just tuberculosis. Using CIMAR as a platform, Dr. Aldridge anticipates she and other researchers will forge collaborations using DiaMOND that could change how a host of different diseases treatments are developed.
One of CIMAR’s core missions is to expand educational efforts around antimicrobial resistance research and surveillance. In 2012, the President’s Advisory Council on Science and Technology raised alarm at the high numbers of early college undergraduates initially interested in science careers, but then leaving those majors for other fields. One of the Council’s recommendations to curb this attrition was to provide students with research opportunities earlier on in their academic careers. Unfortunately, in cases where funds and resources are limited or the student population is high, these research programs are difficult for universities and colleges to implement on their own.
Dr. Carol Bascom-Slack from TU’s Center for Translational Science Education (CTSE), along with colleagues, developed the Prevalence of Antibiotic Resistance in the Environment (PARE)
Program to help solve this problem. PARE partners 125 undergraduate institutions in the United States along with others in Botswana, France, and India. Students participating in PARE’s core module collect soil at a sample site, dilute and plate the soil in the laboratory (with and sometimes without antibiotics), count the colonies of bacteria, and then calculate the percentage of those bacteria that are drug-resistant. When the students, who number in the thousands each year, go to these sample sites, they use a phone application to record their GPS coordinates and other characteristics about the surrounding environment. They also use the app later to upload the data collected in the lab, allowing the PARE team to observe trends and collaborate with other CIMAR faculty to further the research. One example of students’ findings includes preliminary indications of higher AMR levels in soil samples near dog parks and veterinary clinics.
CTSE faculty have also developed projects to engage high school students with the science behind real-world experiences. One such program is the “Great Diseases” project, which focuses on the various diseases that impact quality of life. One of the program’s modules builds upon a landmark 1976 New England Journal of Medicine paper by Dr. Stuart Levy demonstrating the ecologic ramifications of introducing antibiotics into feed for farm animals. Students in the Great Diseases program make analyses and predictions based on an amended version of Dr. Levy’s data.

Dr. Stuart Levy and his wife, Dr. Cecile Levy, open a gift during the Stuart B. Levy, MD Tufts CIMAR Symposium on March 18, 2019. (Alonso Nichols/Tufts University)
Dr. Jay Levy, who is Dr. Stuart Levy’s brother and Director of the Laboratory for Tumor and AIDS Virus Research at the University of California at San Francisco, spoke about how Stuart’s work has continued importance in research and medicine in a broad range of fields. He said that, for example, the lessons learned from antibiotics as described in this article can also be used to inform anti-HIV therapies. HIV, like bacterial pathogens, can become resistant to therapies, and these resistant strains can be passed along to others.
Dr. Ellen Koenig, the Levys’ sister and a founding member of the APUA, discussed the history and continuing importance of the APUA as a global research and advocacy organization in the fight against AMR. Dr. Koenig is a Medical Director of the Instituto Dominicano De Estudios Virologicos in Santo Domingo, Dominican Republic, where antibiotics continue to be overprescribed to human patients and added to livestock feed.
Both Dr. Jay Levy and Dr. Koenig are working to improve healthcare and patient outcomes through their work. Inspired by their brother, they continue to advocate for the prudent use of antimicrobial drugs. “I think one of the most important things Stuart has said is that antibiotics are societal drugs,” said Dr. Levy. “When [resistance] gets into the environment, it affects the whole society and not just the individual.”
Dr. Deborah Kochevar, Provost and Senior Vice President ad interim of Tufts University, and Dr. Harris A. Berman, Dean of the School of Medicine, also spoke at the Symposium to advocate for drug resistance research. Dr. Kochevar emphasized the importance of One Health research and CIMAR’s unique position within Tufts University and Tufts Medical Center as a potential leader in combatting AMR. Dr. Berman agreed. He added that Dr. Stuart Levy’s decades-long commitment to keeping AMR in the spotlight as a global danger is in part what has made these two institutions and now CIMAR important pillars in the fight against drug resistance.
Written by Efrat Hamami, Dr. Wenwen Huo, and Rima Mycynek
Contributions by Dr. John Leong,
Edited by Dr. Bree Aldridge and Rima Mycynek