Center Leadership
Ralph Isberg
PhD | Director
Dr. Isberg has been an acknowledged leader in the field of bacterial pathogenesis for over 30 years, with particular emphasis on pneumonic and diarrheal diseases. He has a major interest in identifying strategies for eliminating drug resistance in nosocomial pathogens, focusing on Acinetobacter baumannii. Among his awards was election to the National Academy of Sciences in 2009.
Dr. Thorpe’s research includes translational work assessing the impact of antimicrobials on human gastrointestinal microbiota and metabolome, with a specific focus on treatment of C. difficile infection. She is interested in how microbial communities shift in response to disease and antibiotic treatments, and how those shifts may predispose to colonization with antibiotic resistant organisms or have other deleterious impacts. She is also interested in host-pathogen interactions with a particular focus on Shiga toxin-producing E. coli.
Bree Aldridge
PhD | Associate Director & Combinatorial Treatment Core Director
Dr. Aldridge leads a multidisciplinary research group coupling quantitative single-cell measurements and mathematical modeling with the goal of shortening and simplifying treatment regimens against tuberculosis. The Aldridge Laboratory merges engineering and molecular approaches to develop quantitative descriptions of the determinants of mycobacterial stress tolerance and virulence.
Brian Noonan
PhD | Executive Director
Dr. Noonan is an experienced leader of interdisciplinary research teams both in academia and industry. He works closely with our faculty to develop grant proposals and is in charge of our outreach to pharma and philanthropy. His research interests include the discovery of vaccines and anti-microbial agents targeting important pathogens and the use of immunomodulatory biologics to control cytokine induction in sepsis.
John Leong
MD, PhD | Senior Leadership
Dr. Leong is Edith Rieva and Hyman S. Trilling Professor and Chair of the Department of Molecular Biology and Microbiology at Tufts University School of Medicine. His research focuses on the interaction of pathogenic Escherichia coli, Borrelia burgdorferi (the Lyme disease spirochete) and Streptococcus pneumoniae with host immune and epithelial cells in order to understand the infectious process and develop novel therapies to prevent or treat these infections.
Debra D. Poutsiaka
MD, PhD | Senior Leadership
Dr. Poutsiaka is Interim Chief of the Division of Geographic Medicine and Infectious Diseases at Tufts Medical Center as well as Professor of Medicine at Tufts University School of Medicine in Boston. Her research interests focus on infections in immunocompromised patients, sepsis, and clinical trials of COVID-19 therapies.
David R. Snydman
MD, FACP, FIDSA, FAST | Senior Leadership
Dr. Snydman has 35 years of experience in observational and interventional studies in translational research, including trials that resulted in FDA licensure of a biologic product. He has worked on epidemiologic aspects of antibiotic resistance for decades, focusing on hospital-acquired infections, anaerobes, C difficile, and MRSA. His current research is focused on the transmission of antibiotic resistance and C. difficile among nursing home patients and in health systems, as well as the impact of antimicrobial stewardship.
Stuart B. Levy
MD | In Memoriam
The name behind our center, Dr. Levy was a trailblazing force in the field of antimicrobial resistance. During his more than four decades at Tufts University and Tufts Medical Center, he led the paradigm shift in how we view antibiotic use and stewardship. In his work on mechanisms of antibiotic resistance and spread of resistance determinants among microbes, his was the first voice of warning of the dangers of antibiotic overuse in the emergence of drug resistance.
Core Faculty
Aimee Shen
PhD
Associate Professor of Molecular Biology & Microbiology, TUSM
My group studies how Clostridioides difficile, a leading cause of antibiotic-associated diarrhea and gastroenteritis-associated death in the United States, forms infectious spores and how these spores germinate upon sensing specific bile salts in the mammalian gut. Spore formation and germination are essential for C. difficile to transmit disease, and analyses of these processes have revealed major differences relative to previously studied spore formers. We use a multi-disciplinary approach to identify regulators of these processes and elucidate their mechanisms of action. A better understanding of the basic biology of C. difficile sporulation and spore germination should facilitate the development of spore-specific therapies that can prevent C. difficile disease transmission. These analyses have also led us to study the mechanisms underlying antimicrobial resistance and responses to physiological stressors in C. difficile and develop methods for visualizing C. difficile’s response to these stressors.
Alysse G. Wurcel
MD
Attending Physician in Geographic Medicine and Infectious Diseases, TMC; Associate Professor of Medicine, TUSM
I am an infectious diseases clincian and and an NIH-funded health disparities researcher. My research interests include prevention and treatment of infection diseases in people who use drugs and people who are incarcerated.
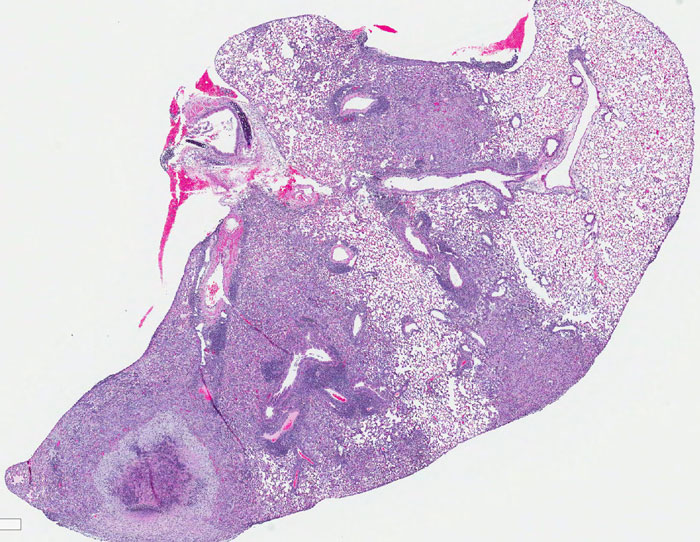
Amanda Jezek Martinot
DVM, MPH, PhD, DACVP
Assistant Professor of Pathology (Anatomy), TUCSVM
I investigate mechanisms by which we can use alternatives to antibiotics such as therapeutic vaccination and host-directed therapies to combat multi-drug resistant tuberculosis. My lab focuses on mycobacterial genetics to identify mycobacterial genes involved in virulence and evasion of the host-immune response, including vaccine responses. By studying TB virulence genes, I hope to identify TB antigens critical for TB survival in the host with the aim to target those TB proteins in vaccine design.
Andrew Camilli
PhD
Professor of Molecular Biology & Microbiology, TUSM
My lab focuses on using bacteriophage therapy against antibiotic-resistant Gram-negative pathogens, primarily Vibrio cholerae, which is the causative agent of cholera.
Benjamin Wolfe
PhD
Associate Professor of Biology, TUSAS; Co-Director of Science, Technology and Society
My lab has been using metagenomic sequencing to identify antibiotic resistance reservoirs in food systems, and we have also been working to identify how microbial interactions could drive the evolution of antibiotic resistance. More broadly, the research in my lab links ecological and evolutionary patterns in microbial communities with the molecular mechanisms that generate these patterns. Using tractable microbial communities from isolated from food systems, we have two broad research goals: identify the molecular mechanisms that control the assembly and function of microbial communities determine how microbial species evolve within multi-species communities. Our work will help develop principles of microbial community assembly that can guide the design and manipulation of microbial communities in agriculture, industry, medicine, and nature.
Berri Jacque
PhD
Associate Professor of Medical Education, TUSM; Director, Tufts University Center for Translational Science Education
Our work at CTSE engages future scientists and citizens in the science of health by fostering collaboration among biomedical scientists and high school educators. One of our projects focuses bring infectious diseases and AMR to high school classrooms across the country to increase science engagement and health literacy.
Brian D. W. Chow
MD
Attending Physician; Director, Infectious Diseases Fellowship Program, TMC; Assistant Professor of Medicine, TUSM
My main work involves clinical trials which advance novel therapeutics and vaccines to FDA approval. I’m interested in trials involving bacteriophage as adjunctive therapy for drug resistant infections. I have also worked on research and quality improvement projects on vaccines and clinical trials for RSV vaccines, RSV prophylaxis, and SARS-CoV-2 therapeutics and vaccines.
Caroline Genco
PhD
Provost & Senior Vice President, Tufts University; Arthur E Spiller Professor of Immunology, TUSM
My translational work has encompassed clinical studies evaluating immunological and microbiological responses following acute inflammatory diseases induced by sexually transmitted infections. Gonorrhea, caused Neisseria gonorrhoeae, is a disease of worldwide prevalence. The continued persistence and increased N. gonorrhoeae resistance to third generation cephalosporins is a warning for the development and spread of untreatable gonorrhea. One of our long-term goals is to develop a vaccine to treat sexually transmitted infections with emphasis on prevention of secondary complications in women.
Carol Bascom-Slack
PhD
Research Assistant Professor of Medical Education, TUSM
My work bridges environmental surveillance with education through a unique tracking program that engages undergraduates and high school students in classroom-based research activities to monitor resistance levels in environmental samples worldwide. Data contributed by students is curated and recorded in a GIS-based mapping system, providing researchers with an overview of potential hotspots of antimicrobial resistance.
Charles Shoemaker
PhD
Professor of Infectious Disease and Global Health, TUCSVM
My research focuses on the development and application of therapeutic biomolecules for treating a variety of diseases caused by pathogens such as C. difficile, Campylobacter, Vibrio cholera and various pathotypes of E. coli. Most of our therapeutic agents employ single domain antibody (sdAb) binding agents consisting of the VH region of heavy-chain-only Abs (VHHs) from immunized alpacas which have been selected for their ability to neutralize critical pathogen functions. These simple, stable VHH agents are then re-engineered in various ways to produce practical, cost-effective products with demonstrated potential to prevent or treat some diseases.
Claire L. Fellman
PhD, DVM
Assistant Professor of Small Animal Internal Medicine & Clinical Pharmacology, TUCSVM
I am a small-animal internist and clinical pharmacologist. I am part of a One Health collaboration with Annie Wayne, a veterinary criticalist at the Cummings School and fellow Levy CIMAR Core Faculty Member, as well as individuals at Tufts Medical Center. Together, we aim to bring human stewardship principles to companion animal veterinary medicine. I am also involved in clinical trials to provide evidence for appropriate antimicrobial treatment durations in veterinary patients.
As of 2023, I am the president-elect for ISCAID (International Society for Companion Animal Infectious Diseases), the group responsible for the most widely used antimicrobial guidelines.
Clay Bennett
PhD
Associate Professor of Chemistry, TUSAS
Research in my lab focuses on the synthesis of oligosaccharide antibiotics. These include compounds with broad spectrum activity against gram negative bacteria, as well as molecules that target Group B strep (GBS).
David M. Gute
MPH, PhD, FACE
Professor of Civil & Environmental Engineering, TUSE
The working title of the doctoral dissertation of Kate Woodward, P.E., who I advise is “Removal of Antibiotic Residues and Control of Antibiotics Movement from Cattle Industry Wastewater in Nebraska.” Antibiotics used in livestock production to treat and prevent infections may impact human health by promoting development and excretion of resistant bacteria or genes in animal manure.
Elena N. Naumova
PhD
Professor and Chair of the Division of Nutrition Data Sciences, TUFSN
Adjunct Professor of Civil and Environmental Engineering, TUSE; Public Health & Family Medicine, TUSM, Mathematics, TUSAS
Emerging and re-emerging diseases, environmental epidemiology, molecular biology, nutrition, and growth
Fiorenzo Omenetto
PhD
Frank C. Doble Professor of Biomedical Engineering; Dean of Research, TUSE
My research interests are in the convergence of technology, biologically inspired materials, and the natural sciences with an emphasis on new transformative approaches for sustainable materials for high-technology applications.
Gabriela Andujar Vazquez
MD
Attending Physician, TMC; Assistant Professor, TUSM
I am the Associate Director for the Antimicrobial Stewardship Program at Tufts Medical Center. My areas of interest are antimicrobial stewardship in long-term care facilities (LTCFs), hospital-acquired infections, diagnostic stewardship and rapid diagnostics in infectious diseases as well as continuing partnerships with public health authorities in order to tackle antimicrobial resistance.
Helen Boucher
MD, FACP, FIDSA
Dean, TUSM; Chief Academic Officer for Tufts Medicine
My clinical interests include infections in immunocompromised patients and S. aureus infections, and my research interests focus on S. aureus and the development of new anti-infective agents. (Note: Dr. Boucher was Director of the Levy CIMAR along with Dr. Ralph Isberg from 2018-2021. Her work in antimicrobial resistance extends to education, policy, outreach, and more. She is a Fellow and Member of the Board of Directors of the Infectious Diseases Society of America, and is appointed to the Presidential Advisory Council on Combating Antibiotic-Resistant Bacteria, or PACCARB.)
Honorine Ward
MD
Professor of Medicine, TUSM and TMC
The intestinal parasite Cryptosporidium, (which is resistant to most antimicrobials including the classic antifolate antiparasitic drugs), is a major cause of diarrheal disease worldwide, particularly in immunocompromised hosts such as untreated patients with HIV/AIDS and malnourished children in resource-limited settings. Our research is focused on: 1) understanding the pathogenesis of human Cryptosporidium infection using novel bioengineered 3D intestinal tissue models; 2) the molecular basis of Cryptosporidium-host cell interactions, seeking to investigate proteins which mediate these interactions and enzymes that post-translationally modify them; 3) immune responses to Cryptosporidium in children in resource-limited settings where cryptosporidiosis is endemic; and 4) the intestinal microbiome in infectious diarrheal disease including childhood cryptosporidiosis and malnutrition. 5) understanding of recovery after post-acute sequelae of SARS-CoV-2 infection in adults.
Husain Poonawala
MBBS, MPH
Attending Physician; Assistant Director of the Clinical Microbiology Laboratory, TMC
My research focuses on tuberculosis and non-tuberculous mycobacteria, and I am interested in studying how next-generation sequencing and novel diagnostic methods can be integrated into clinical care and public health interventions that can be used to improve outcomes from these infections.
Irene Georgakoudi
PhD
Professor of Biomedical Engineering, TUSE
Tissue engineering and cancer diagnostics
Joan Mecsas
PhD
Professor of Molecular Biology & Microbiology, TUSM
My lab investigates factors required for Klebsiella pneumoniae to cause disease in lungs, blood, liver and bladder, as well as genetic, host-derived, and chemical factors that render multi-drug resistant Klebsiella more susceptible to treatment.
Jonathan A. Runstadler
DVM, PhD
Professor of Infectious Disease and Global Health, TUCSVM
My lab seeks to understand genetic factors that impact susceptibility to infectious disease, specific or general and the repercussions for potential epidemics, persistence, and evolution of those infectious agents. Using a combination of our own field samples, collaborations and published genomic data, we are developing tools to investigate correlates of influenza disease resistance and/or susceptibility among multiple species. We seek to provide unbiased host factors associated with viral resistance/susceptibility while contributing valuable tools for all investigators.
Kap Sum Foong
MD
Attending Physician in Geographic Medicine and Infectious Diseases, TMC; Assistant Professor of Medicine, TUSM.
I am an infectious diseases clinician and clinical researcher. My research interests include antimicrobial and diagnostic stewardship in acute care, long-term care, and OPAT (outpatient parenteral antimicrobial therapy) care settings.
Kenneth Kaitin
PhD
Professor & Director, Tufts Center for the Study of Drug Development
My group studies the economic, political, technical and scientific challenges of developing new antimicrobials and other pharmaceutical products. We also examine how regulatory policy influences innovation in areas of unmet medical need, such as AMR.
Krishna Kumar
PhD
I am interested in the molecular design of structural scaffolds for discovering new antimicrobial compounds especially those against resistant organisms, as well as the use of organic chemistry, biological chemistry, biophysics, and cellular biology to understand mechanism of action of therapeutically relevant antibiotics.
Kyongbum Lee
PhD
Dean Ad Interim and Karol Family Professor of Chemical and Biological Engineering; Tissue and Metabolic Engineering Laboratory, TUSE
My research interests include metabolic engineering, tissue engineering, and systems biology, as well as the study of cellular metabolism and its role in shaping biological function. A major ongoing effort is to investigate metabolites that mediate chemical communication between bacterial gut microbiota and the host.
Linden Hu
MD
Paul and Elaine Chervinsky Professor in Immunology and Vice Dean for Research, TUSM
The focus of my research is on Lyme disease. My laboratory is interested in the pathogenesis of Lyme disease both from the perspective of how the bacteria adapt to its different host environments as well as how the host immune response recognizes the organism and is responsible for the pathology associated with the infection. As a physician scientist, my overall goals are to be able to improve prevention, treatment and diagnosis of human Lyme disease and to this end, we have been working on projects to develop vaccines and improved diagnostics for the presence of disease after antibiotic therapy. We are working in the area of antibiotic development to develop narrow spectrum agents for Lyme disease that will limit the development of resistance in off-target bacteria by ensuring that most other bacteria are already naturally resistant.
Marieke H. Rosenbaum
DVM, MPH, MS
Research Assistant Professor, TUCSVM
My research focuses on understanding how domestic and wild animals such as backyard chickens and city rats contribute to the spread of AMR genes in urban centers.
Majd Alsoubani
MD
Fellow in Geographic Medicine and Infectious Diseases, TMC
My main clinical and research interests focus on antimicrobial stewardship and resistance in solid organ transplant recipients. My research focuses on the impact of Clostridioides difficile resistance and ribotypes on clinical outcomes especially in patients with immunocompromising conditions.
Maureen Campion
PharmD, BCIDP
Senior Clinical Pharmacy Specialist in Infectious Diseases, TMC
I am the senior pharmacist responsible for antimicrobial stewardship and ID consult services Tufts Medical Center. I serve as a preceptor and lecturer for pharmacy residents and ID fellows. My research interests include clinical and economic outcomes associated with antimicrobial stewardship.
Michael R. Jordan
MD, MPH
Attending Physician, TMC;
Assistant Professor, TUSM
I study HIV drug resistance and translate results into public health and antiretroviral therapy program policy in low- and middle-income countries. In addition, my laboratory studies inter- and intra-host diversity of SARS-CoV-2 and SARS-CoV-2 antiviral drug resistance.
Nikhil Nair
PhD
Assistant Professor of Chemical & Biological Engineering, TUSE
The Nair lab is interested in using the tools of synthetic and chemical biology to understand the effect of antimicrobials on the structure and function of microbial communities.
Peter Gwynne
PhD
Research assistant professor, TUSM; Director for Translational Research, Tufts University Lyme Disease Initiative
I study the molecular mechanisms the bacterium Borrelia burgdorferi, which causes Lyme disease, uses to transition between different hosts such as ticks, mice, and humans. My research aims to exploit these unique metabolic interactions to design targeted drugs for Lyme disease.
Qiaobing Xu
PhD
Associate Professor of Biomedical Engineering, TUSE,
Associate Professor, TUSM
Developing synthetic materials for the delivery of therapeutic biomacromolecules
Revati Masilamani
PhD
Assistant Professor of Medical Education, TUSM
I serve as Director of the Lab Science Investigators Program on AMR, Director of the Great Diseases curriculum, and Co-Director of the Mini-Med Connect Programs for pre-college learners at the Center for Science Education at Tufts University. I also teach immunology in the professional programs at Tufts University School of Medicine. After my doctoral work in Immunology and a postdoctoral fellowship in Infectious Disease, I trained in curriculum design and evaluation in the domain of biomedical education. I have experienced science education from the prism of having designed curriculum for, and teaching, a wide spectrum of learners from high school students, K-12 educators, medical students, and graduate students. My research focuses on models to strengthen engagement with science and health awareness in adolescent populations through inclusive, equitable teaching practices.
Sankha (Bobby) Basu
MD, PhD
Director of Clinical Microbiology, TMC
My research is focused on the design and development of novel mass spectrometry-based approaches to diagnose and study infectious disease, cancer and drug distribution.
Shira Doron
MD
Attending Physician, Associate Hospital Epidemiologist, and Antimicrobial Steward, TMC; Professor of Medicine, TUSM
My research focuses on the implementation of antimicrobial stewardship strategies in human acute care, human long term care, and animal care settings.
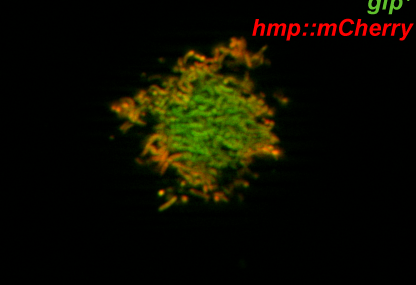
Shumin Tan
PhD
Assistant Professor of Molecular Biology & Microbiology, TUSM
My lab’s research centers on understanding how Mycobacterium tuberculosis exploits environmental cues to survive and grow in its host. As part of this focus, we seek to (i) elucidate regulatory nodes that enable the bacterium’s coordinated response to disparate cues and that thus represent novel therapeutic targets in both drug-sensitive and drug-resistant bacteria, and (ii) understand how microenvironment heterogeneity impacts infection outcome and treatment efficacy.
Trever Smith
PhD
Research Assistant Professor, TUSM
In my research, I use a combination of fluorescence microscopy, omics style data, and computational biology to understand how drugs target and kill Mycobacterium tuberculosis (Mtb). Using antibacterials to inhibit specific cellular processes, I am currently investigating how perturbations to one or more pathways contribute to Mtb cell death.
Yoav Golan
MD, FIDSA
Associate Professor of Medicine, TUSM; Attending Physician, TMC
I investigate the risk factors for infections by antibiotic-resistant organisms and develop scores to target certain patients for therapy for such organisms. My research focuses on infections by resistant Gram negative pathogens, C. difficile, and other hospital-acquired pathogens.
Affiliate Members
Amy Pickering
PhD
Assistant Professor of Environmental Engineering, UC Berkeley
Web | Twitter
Our lab studies environmental and zoonotic transmission of antibiotic resistance, primarily in low-income countries, with an aim to develop strategies to prevent early life exposure to antibiotic resistant pathogens. I serve as the Blum Center for Developing Economies Distinguished Chair in Global Poverty and Practice at Berkeley.
Anders P. Håkansson
PhD
Professor of Infection Medicine, Lund University, Sweden
Web | Twitter
My laboratory focuses on understanding host-pathogen interactions, with emphasis on respiratory pathogens, using this knowledge to develop novel preventive and therapeutic strategies to protect against bacterial infection. Our work focuses on both the factors used by bacteria to establish colonization and cause disease and how this is counteracted by the host inflammatory response to colonization and infection. We are working on several major research projects, including the study of the direct bactericidal activity of a human milk protein-lipid complex against various bacterial species as well as its adjuvant activity in sensitizing bacteria to a broad range of common antibiotics to provide novel therapeutic strategies against respiratory and other infections with antibiotic-resistant bacteria.
Edward Geisinger
MD, PhD
Assistant Professor of Biology, Northeastern University
Web | Twitter
Our lab investigates the molecular basis of antibiotic resistance and disease development in infections with hospital-acquired pathogens. Our primary focus is the troublesome microbe Acinetobacter baumannii, a frequent cause of pneumonia and sepsis in intensive care units that has developed resistance to virtually all clinically useful antibiotics. We examine unique strategies used by the pathogen to build and fortify its cell envelope, including regulatory networks hardwired to amplify resistance and virulence upon detection of antimicrobial stress. We employ a variety of tools ranging from systems biology and molecular genetics to animal models of infection. Long-term, we will exploit these strategies as targets for novel therapies against nosocomial diseases.
Mark L. Nelson
PhD
Vice President of Business & Science Development, Echelon Biosciences, Inc. and Frontier Scientific, Inc.
Webssite (Wikipedia)
I work in the areas of drug discovery, medicinal chemistry, and the development of therapeutic agents, a career which began in 1987 during my postdoctoral training under Dr. Stuart Levy at Tufts University. I joined Paratek Pharmaceuticals, inc., cofounded by Dr. Levy and Harvard’s Dr. Walter Gilbert, at its inception in 1996, and we created over 3,000 new derivatives of the tetracycline family of chemotherapeutics that resulted in clinical compounds progressing towards commercialization. The drugs Nuzyra and Seysara were FDA-approved in 2018 for severe infections, anthrax and severe acne, and our team won the American Chemical Society Heroes of Chemistry award in 2019 for this work. My current research is directed at modulating alpha-proteobacteria and related mitochondria and their signaling processes, and new compounds are in pre-clinical studies affecting activated immune cells showing promise against the secondary effects of stroke, hypoxia and neurodegeneration. I hold over forty patents and have numerous publications and reviews in the areas of drug design, antibiotics, and drug discovery.
Maya Nadimpalli
PhD
Assistant Professor, Gangarosa Department of Environmental Health,
Rollins School of Public Health, Emory University
Web | Twitter
I use genomic and epidemiological approaches to understand how exposures to food, animals, and the environment can impact human colonization and infection with antibiotic-resistant bacteria, particularly in low-resource settings. Currently, I am exploring whether nutritional or behavioral interventions could improve young children’s gut colonization resilience against resistant pathogens.
Muhammad Zaman
PhD
Professor of Biomedical Engineering and Global Health, Boston University
Web | Twitter
Our lab’s research in the global health arena focuses on antimicrobial resistance, One Health integrated solutions and improved testing of drug quality in relations of health equity and antimicrobial resistance. Our work in the lab works closely with work in the field and in the policy domain for rich understanding and efficient implementation. Recent work has also focused on access to better healthcare for refugees and marginalized populations and the role engineers can play in improving the health of the most vulnerable people. Our students come from not just engineering but also public health, social sciences and humanities to collectively address some of the most pressing global problems in access to health and health equity. We are also interested in issues of science literacy and broader engagement of the public. My recent book, “Biography of Resistance,” is an effort in that direction.
Tim van Opijnen
PhD
Associate Professor of Biology, Boston College
Web | Twitter
Our lab focuses on the development and application of experimental and computational Systems Biology tools to study infectious diseases as complete systems while in interaction with their environment (e.g. the host and/or drugs). Our ultimate goal is to develop approaches to predict and detect the emergence of (drug-resistant) infectious diseases and strategies to eradicate them. To achieve this, we employ a unique mixture of approaches from the fields of Biology, Chemistry, Physics and Computer Science, including a variety of sequencing strategies, microfluidics, robotic automation, immune system monitoring, in vivo disease models, computational modeling and machine learning.



































![REB_8103[69]](https://www.tuftscimar.org/wp-content/uploads/2022/12/REB_810369-150x150.jpg)