CIMAR Joins the Battle Against AMR with Collaborative and Brainstorming Workshop

January 21, 2019
The Tufts Center for Integrated Management of Antimicrobial Resistance (CIMAR) hosted its first event last month to introduce the Center to the local scientific community and to offer a platform for investigators and clinicians to showcase their research and promote collaborations. CIMAR aims to address the rise and spread of antimicrobial resistance (AMR), and we believe our faculty possess the myriad unique skillsets needed to lead this fight. Roughly 700,000 human deaths are attributable to AMR each year globally, and if trends continue, AMR could contribute to a total of 350 million deaths by 2050.
CIMAR will address AMR through a multidisciplinary approach around themes of combination drug therapy, surveillance and stewardship from a One Health vision, and education. The Center has received funding from both Tufts Medical Center (TMC) and the Tufts University School of Medicine (TUSM) to support platform development, seminar series, symposia, workshops, seed grants, and industry collaborations.
To this end, Dr. Tracy Schmidt, Associate Director for Corporate & Foundation Relations, introduced “Tufts@Kendall” in collaboration with the Massachusetts Biotechnology Council (MassBio). Tufts@Kendall is envisioned as an environment where scientists and members of industry can meet to discuss funding and collaboration for the advancement of science.
Though the more than 20 researchers who spoke at CIMAR’s workshop presented on numerous fascinating areas of AMR-related science and policy, the overarching themes of the day can be categorized into four groups:
Combination Therapy and Drug Development
Combinatorial drug therapies are crucial in treating infections and will be key in diminishing the emergence of AMR in humans and animals.
Dr. Kenneth Kaitin from the Tufts Center for the Study of Drug Development kicked off the first session of talks. He pointed out that anti-infective agents (not limited to antibiotics) suffer from a low competitive advantage in the current drug market. Dr. Kaitin suggested that a combination of “push and pull” regulatory and legislative initiatives could boost incentives to develop new anti-infective drugs and increase the number of clinical compounds that obtain approval by the Food and Drug Administration and reach the market.

TUSAS’s Dr. Clay Bennett, whose work includes targeting the bacterial “glycome” with antimicrobial oligosaccharides, answers questions for TUSE and TUSM’s Dr. Bree Aldridge (© 2018 Dr. Claudette Gardel for CIMAR)
Workshop participants also presented on drug and combination therapy development. Dr. Clay Bennett (Tufts University’s Department of Chemistry) targets the bacterial “glycome” with antimicrobial oligosaccharides, including some previously identified compounds that fell out of clinical trials but may have potential once the important components of the oligosaccharide are identified.
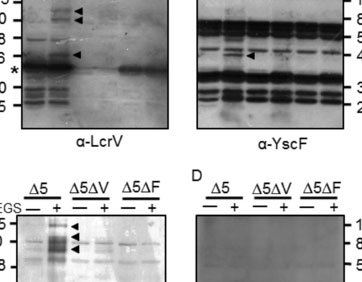
Dr. Edward Geisinger (Northeastern University’s Department of Biology) described a genome-wide approach to studying drug-resistant Acinetobacter by combining Tn-Seq and CRISPRi to measure stress responses to sub-lethal drug concentrations and identify unknown genes involved in drug resistance. Dr. Bree Aldridge (Tufts University’s Departments of Molecular Biology & Microbiology and Biomedical Engineering) described a new method called DiaMOND to systemically study pairwise and high-order drug combinations to develop shorter, more efficient treatment regimens for bacterial infections. Dr. Joan Mecsas (Tufts University’s Department of Molecular Biology & Microbiology) proposed targeting bacterial-specific biosynthetic pathways with small molecules or compounds as a combination therapy for Klebsiella pneumoniae infections.
Antimicrobial Resistance in Hospitals and Antibiotic Stewardship:
Antimicrobial stewardship is a crucial element in the fight against AMR. It promotes the appropriate use of antimicrobial agents and is known to improve patient outcomes as a result.
Dr. David Snydman (Chief of the Division of Geographic Medicine and Infectious Diseases at TMC) highlighted the epidemiologic aspects of hospital-acquired infection and some of the work that is being done at TMC to study the interaction between Vancomycin-resistant enterococci (VRE), Clostridium difficile, and the microbiome. He also emphasized the importance of understanding the spread of AMR organisms throughout the healthcare system (including long-term care and nursing homes) as well as increasing education and antibiotic stewardship in healthcare systems outside of hospitals.

Dr. Kirthana Beaulac from TMC’s Antimicrobial Stewardship Leadership Team, asks a Tufts University investigator about her research methodology (© 2018 Dr. Claudette Gardel for CIMAR)
Dr. Anne Kane (TMC’s Phoenix Laboratory) described how the use of narrow-spectrum antibiotics decreased susceptibility of patients to C. diff infection compared to more commonly used broad-spectrum antibiotics, which create large microbiome changes and make patients susceptible to infection.
Drs. Shira Doron, Kirthana Beaulac, and Gabriela Andujar Vazquez of Tufts Medical Center’s Antimicrobial Stewardship Program Leadership Team promoted the proper clinical use of antibiotics and highlighted the strides that TMC has made in antibiotic stewardship since implementing the program in 2003. The program performs better than local and national benchmarks in antimicrobial usage, and as a result, TMC is the only hospital in the northeastern United States to have received the IDSA Center of Excellence designation. The antimicrobial stewardship group uses daily surveillance on an individual patient level and is working in collaboration with the Massachusetts Department of Public Health to bring these techniques into long-term care and nursing home settings.
Dr. Annie Wayne, (Tufts University’s Cummings School of Veterinary Medicine), who also presented with this group, discussed human-to-pet transmission of AMR microbes. Dr. Wayne is working to implement antibiotic stewardship best practices in veterinary hospitals.
Basic Science and Engineering Research — Tackling Multidrug Resistant Infections:
Researchers from both the School of Medicine and the School of Engineering at Tufts University are developing tools and techniques to accelerate the understanding of antibiotic resistance. They are also working to translate new treatments and diagnostics in the clinic.
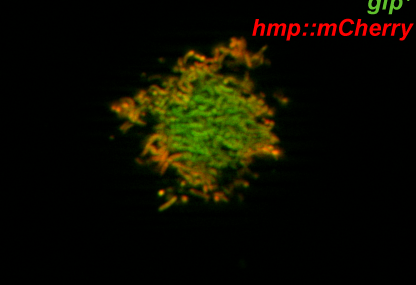
Dr. Andrew Camilli (Department of Molecular Biology & Microbiology) described the potential of using Vibrio cholerae-specific phages to treat family members of cholera patients upon admission of an index case to a hospital setting, thus preventing the spread of cholera through households. Dr. Qiaobing Xu and his group (Department of Biomedical Engineering) have synthesized a proprietary combinatorial library of cationic lipid-like materials as drug carriers to screen for organ-targeted delivery and presented a case study using liposomes to treat fungal infections. Dr. Nikhil Nair (Department of Chemical and Biological Engineering) is using bacteria-specific bacteriocins as molecular probes. This includes using fluorophore-conjugated bacteriocins to live-label bacteria in a population and assess bacteriocin binding vs. killing.
Dr. Irene Georgakoudi (Department of Biomedical Engineering), who studies metabolism using label-free, high-resolution imaging showed how bacterial metabolism in different tissues or after drug treatments can be visualized. Together, these talks highlighted how new imaging techniques may be used to accelerate how we study and diagnose bacterial pathogens. Dr. Giuseppina Matzeu (Department of Biomedical Engineering) presented on how silk and inks can be used for the controlled delivery of antibiotics to develop rapid diagnostics.
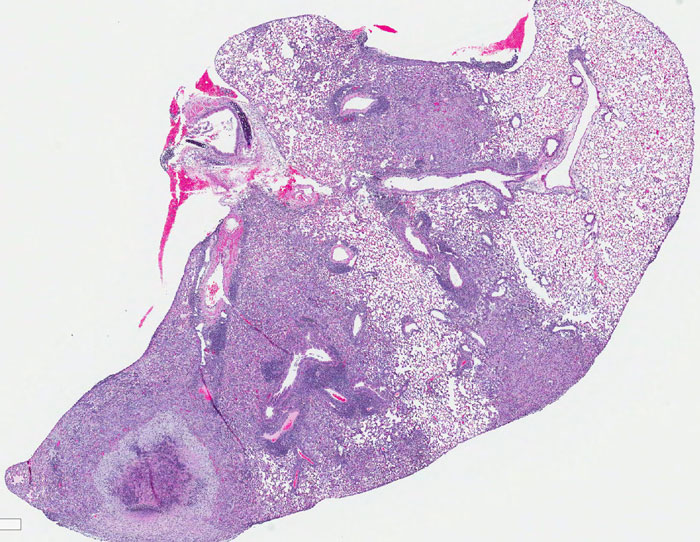
Closing out the session, Dr. Gillian Beamer (Tufts University’s Cummings School of Veterinary Medicine) presented data that even antibiotic-sensitive Mycobacterium tuberculosis can invade stem cells and evade treatment. She proposed studying the stem cell niche using in vitro modeling to better treat TB infections.
Environmental Surveillance and Educating the Public
Surveillance of antimicrobial resistance includes the tracking, sharing, and analysis of data on AMR microorganisms. Findings can prevent outbreaks and can inform clinical therapy choices.

TUSE’s Dr. Amy Pickering describes use of surveillance from water samples to characterize AMR in areas with different water management strategies. (© 2018 Dr. Claudette Gardel for CIMAR)
Environmental surveillance and clinical trials studying the transmission of AMR microorganisms is an important mission for CIMAR and for several of the Tufts University faculty who presented at the workshop. Dr. Amy Pickering (Department of Civil & Environmental Engineering) is conducting environmental surveillance in India using portable DNA sequencing that can both genotype and assign likely AMR profiles using one long DNA read. She is also studying AMR colonization in populations exposed to chlorinated and unchlorinated drinking water and human-to-animal transmission in developing countries.
Dr. Maya Nadimpalli (Department of Civil & Environmental Engineering) described her work studying animal-to-human transmission of multidrug-resistant bacteria in Cambodia, and how resistant bacteria found in food could colonize or mix with other bacteria in the gut, particularly with respect to mobile genetic elements.
In a partnership with a clinic in Nanjing, China, Dr. Caroline Genco (Department of Immunology) studies AMR Neisseria infections and tracks disease transmission between infected men and asymptomatic women using whole RNA-seq to understand gender-specific gene expression that may explain the relative prevalence of asymptomatic infections in women as compared to men. These research efforts are well complemented by CIMAR’s emphasis on education.
Dr. Carol Bascom-Slack from the Tufts University Center for Translational Science Education described how the Prevalence of Antibiotic-Resistance in the Environment (PARE) project can be used to both teach students about AMR and collect data on drug-resistant microorganisms from environments around the United States. PARE is an undergraduate-focused research program where students can analyze soil samples and genotypes, and screen bacteria for drug resistance. PARE and similar programs bring bench research to students while also disseminating important public health messages.
Through this successful workshop, we have shown that CIMAR is already bringing basic scientists and clinicians together and starting important discussions about the problems we face when dealing with AMR. Through freely exchanging ideas and showcasing research, the workshop introduced to the center and to participants a broad overview of the various skill sets available to all those involved in the fight against antimicrobial resistance.
Article by Drs. Anne McCabe and Trever Smith, both postdoctoral scholars in the Department of Molecular Biology & Microbiology, Tufts University School of Medicine
Contributions and editing by Dr. Bree Aldridge and Rima Mycynek
© 2018 Dr. Claudette Gardel for CIMAR