Professor Kevin Outterson Speaks on Bridging Economics, Health Equity, and Scientific Research in the Fight Against AMR
Kevin Outterson, a professor of health law, ethics and human rights at Boston University, spoke at The Fletcher School’s annual Dr. Maurice S. Segal Lecture on Feb. 29. Outterson’s talk, titled“The Social Ecology of Antimicrobial Resistance,” focused on the science, economics and accessibility of antimicrobial medicines. A longtime friend of the Levy CIMAR, Outterson is also the founding executive director and principal investigator of Combating Antibiotic-Resistant Bacteria Biopharmaceutical Accelerator, or CARB-X, a global nonprofit partnership whose mission is to accelerate the development of antibiotics, vaccines and other products that fight against lethal bacteria that have grown resistant to the current circulation of antibacterial products.
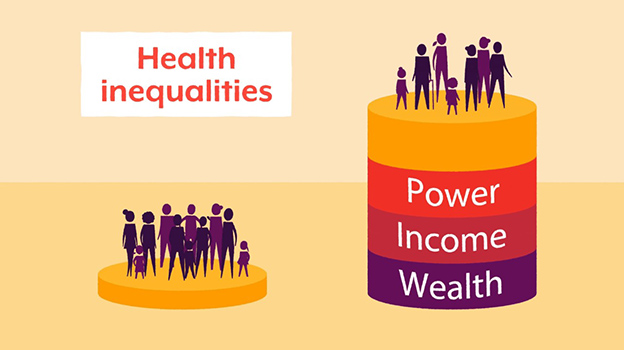
Jacinda C. Abdul-Mutakabbir Explores The Intersection Of Racism, Antimicrobial Resistance, And Vaccine Equity
UC San Diego’s Jacinda Abdul-Mutakabbir, PharmD, MPH, AAHIVP presented on “The Intersection of Racism, Antimicrobial Resistance, and Vaccine Equity” for a Black History Month seminar, focusing on healthcare disparities observed across racially and ethnically minoritized groups. The talk was sponsored jointly by the Levy CIMAR, the Tufts Department of Molecular Biology and Microbiology Diversity, Equity, & Inclusion committee, and the Tufts Graduate School of Biomedical Sciences. Dr. Abdul-Mutakabbir is an Assistant Professor of Clinical Pharmacy at UC San Diego’s Skaggs School of Pharmacy and Pharmaceutical Sciences and in the Division of the Black Diaspora and African American Studies.
Silk Provides the Building Blocks to Transform Modern Medicine
One of the things that sets silk apart as a material is how benign it is. The liquid mixture the researchers start with is essentially just silk fibroin (the core protein in silk) and water—it’s nontoxic and chemically neutral. That means it’s easy to add bioactive molecules such as antibiotics or enzymes. Moreover, silk is remarkably good at stabilizing those molecules and keeping them from degrading. For example, the researchers found that blood samples mixed and dried with silk fibroin remained stable at high temperatures for multiple months. They have had similar findings with vaccines—another spinout company, Vaxess, is currently working to develop silk-based vaccine patches for wide-scale use.
Without a Plan to Fight Superbugs, the Cancer Moonshot Will Never Achieve Liftoff
Researchers at the National Institutes of Health recently outlined strategies to tackle President Biden’s Cancer Moonshot initiative, which aims to cut cancer deaths in half over the next 25 years. They made one glaring omission: a plan to combat drug-resistant superbugs. The two public health crises — cancer and drug-resistant infections — are deeply intertwined. Patients with cancer are three times more likely to die of an infection than patients without the disease. Unless we quickly mobilize to fight superbugs, the Cancer Moonshot will never achieve liftoff.
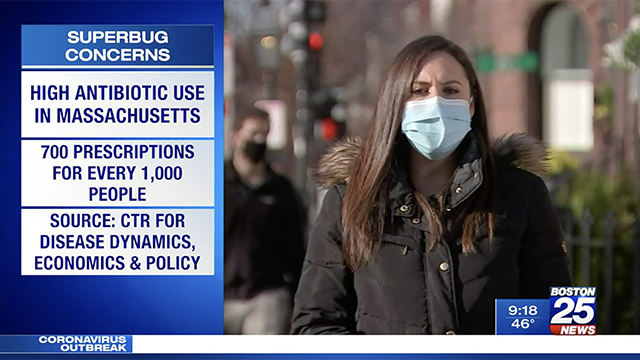
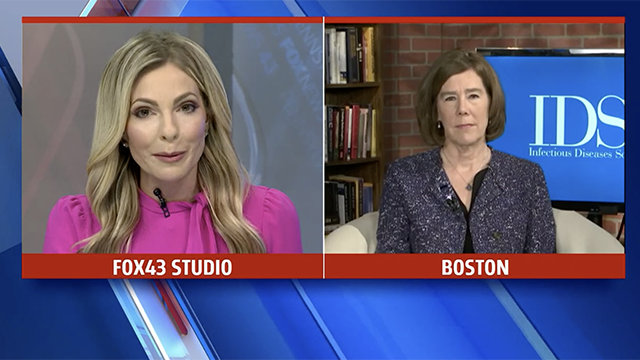
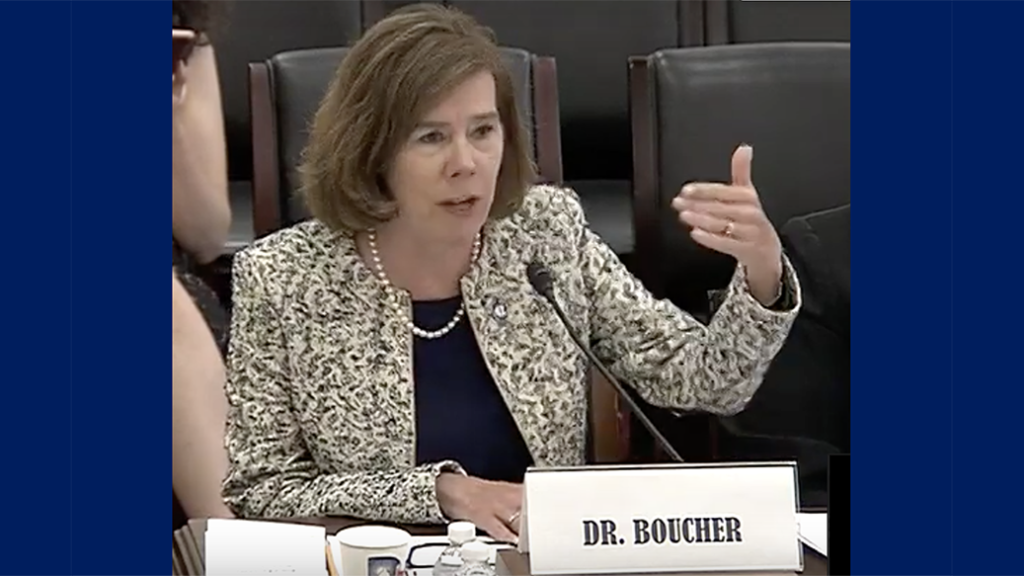
Congress Aims to Tackle Antibiotics Time Bomb
The world’s population is becoming increasingly resistant to antibiotics, and healthcare institutions are sounding the alarm that inaction could result in a breakdown of healthcare systems worldwide within the next 30 years. In 2021, the World Health Organization named antimicrobial resistance as one of the top 10 emerging threats to global health, but lawmakers in the United States have been unable to pass legislation to address the crisis. Levy CIMAR Founding Director and Dean of Tufts School of Medicine, Helen Boucher, MD, spoke on the urgency for Congress to address AMR seriously. She said, “this is a game where there needs to be planning in advance for the threats we know and some we don’t know.”
Overuse of Antibiotics Leading to Dangerous ‘Superbugs’ Examined by U.S. Senate panel
Massachusetts Democratic Sen. Ed Markey, chair of the panel, said that everyone must use antibiotics responsibly. “Antibiotics alone have extended our average lifespan by 23 years,” Markey said. “But the rise in antimicrobial resistance threatens to undo 100 years of medical progress.” Dr. Helen Boucher, Levy CIMAR Founding Director as well as Dean and Professor of Medicine at Tufts University School of Medicine, urged the committee to pass a bipartisan bill already introduced this Congress and called on the Biden administration to appoint someone to oversee issues related to antibiotic resistance.
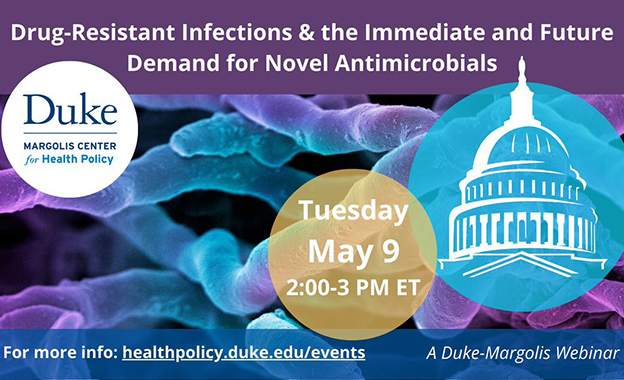
Drug-Resistant Infections & the Immediate and Future Demand for Novel Antimicrobials
Tufts University School of Medicine Dean and Levy CIMAR Founding Director Helen Boucher, MD, joined congressional policymakers, federal policymakers, and other stakeholders interested in addressing drug-resistant infections and antimicrobial resistance (AMR) for an expert panel discussion at Duke University. The panel discussed topics including the current and future threat of drug-resistant infections and antimicrobial resistance, market uncertainties that complicate antimicrobial development and commercialization, and existing and proposed incentives for novel antimicrobials, including the PASTEUR Act.
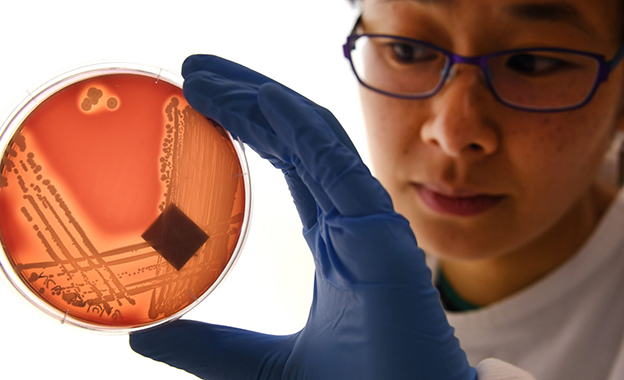
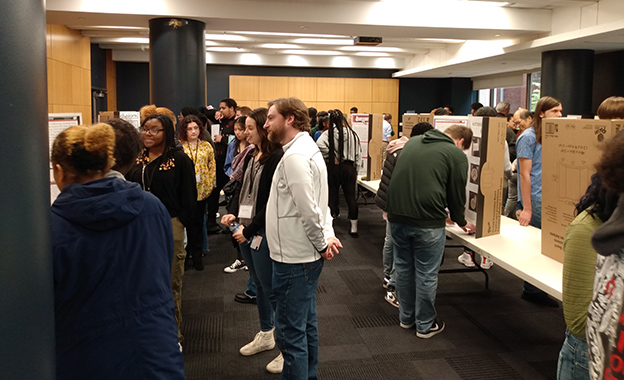
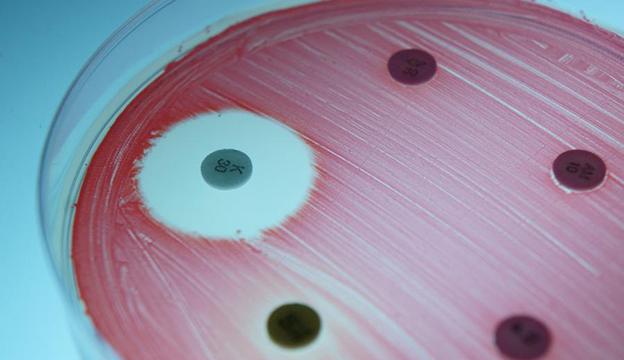
Superbugs From Their Backyards and Beyond: Brockton High Schoolers Present “Tiny Earth” Findings to Levy CIMAR; Tufts Community
The Levy CIMAR hosted 73 students from Boston-area Brockton High School last week for a scientific poster session where the students presented their unique findings after surveilling antimicrobial resistant (AMR) bugs in their own backyards and around Brockton, and culturing them in the lab. The findings the students presented are part of the Tiny Earth project, a research course originally designed by University of Wisconsin-Madison faculty for college students to discover antibiotics from soil bacteria. Brockton is the first public high school in the country to adopt the curriculum.
High Schoolers Become Scientists in Tufts Lab Science Investigations Summer Course on Antimicrobial Resistance
As student researchers in Lab Science Investigations: Antimicrobial Resistance, high schoolers will have a uniquely immersive experience with the One Health approach that recognizes that the health of people is closely connected to the health of animals and our shared environment. In the case of AMR, excessive use of antibiotics in agriculture, animals, and people, all contribute to this problem.. To address this, as part of the STEM Research Institute, students will hear perspectives from experts in many fields and will work with laboratory research techniques used by engineers, social scientists, biomedical scientists, veterinarians, physicians, drug developers, epidemiologists, healthcare policy experts, and environmental scientists, who work together at the Tufts Levy Center for Integrated Management of Antimicrobial Resistance (CIMAR).
Levy CIMAR Awarded $5.15 Million NIH Biomedical Research Facilities Grant
The Levy CIMAR has been awarded a $5.15 million grant from the National Institutes of Health to construct a new biomedical research facility in the Biomedical Research and Public Health Building on the Tufts Health Sciences campus in Boston. The Laboratory for Combinatorial Drug Regimen Design for Resistant and Emerging Pathogens (LCDRD) will provide a modern, centralized laboratory and collaboration space for the Levy CIMAR’s multi-institutional effort to generate novel drug therapies for known and emerging pathogens resistant to current therapies. The new facility will be shared by teams of interdisciplinary researchers from seven Tufts University schools, including the School of Medicine, and Tufts Medicine, as well as collaborators from other regional and national institutions.
How to Stay Safe as Respiratory Illnesses Make Their Rounds
Respiratory illnesses are making the rounds just in time for the holiday season. But after several years apart, families are ready to gather again. With Flu, COVID and RSV all circulating, doctors caution any gathering requires thought and preparation, CBS News reports. “I think it’s really all about your tolerance for risk. There is no such thing as a risk-free gathering,” said Dr. Helen Boucher, Dean of Tufts Medical School and the Chief Academic Officer of Tufts Health. According to Dr. Boucher, the best thing you can do for your family right now is get the flu vaccine and latest COVID booster.
Levy CIMAR Founding Director Helen Boucher Named Dean of Tufts University School of Medicine; CAO of Tufts Medicine
Levy CIMAR Founding Director Dr. Helen Boucher, an expert in infectious disease and antimicrobial resistance, has been named the new dean of Tufts University School of Medicine. The first woman to lead the School of Medicine in its 129-year history, with this appointment Boucher builds on a 20-year career at Tufts as a clinician, professor, administrator, and researcher. She had served as the school’s dean ad interim since last summer, when she was also named chief academic officer for Tufts Medicine, which is the parent health system of Tufts Medical Center, the School of Medicine’s principal teaching-hospital affiliate.
Antimicrobial Stewardship in Jails and Prisons: When Will Then be Now?
Antibiotics save lives, but whenever they are used, they can also contribute to the development of antimicrobial-resistant (AMR) infections, making antibiotics and similar drugs ineffective against the microorganisms they were created to fight. Infections of all kinds—tuberculosis, dental infections, HIV, sexually transmitted infections, COVID-19, and more—are common in jails and prisons, making these facilities places where antibiotics are frequently prescribed. Unfortunately, sometimes antibiotics are prescribed even though they are not clinically indicated, the wrong antibiotics are prescribed, or antibiotics are prescribed for too long.
Cummings School of Veterinary Medicine recruiting patients for UTI clinical trial
Cummings School of Veterinary Medicine at Tufts University (Cummings School) is now recruiting canine patients for a clinical trial testing a 3-day antibiotic treatment for urinary tract infections (UTI). According to an organizational release, researchers in this study are conducting a randomized, placebo-controlled trial to determine if 3 days of the antibiotic amoxicillin is as effective as 7 days for the treatment of UTIs in dogs. The researchers at the Cummings School are hoping if the results verify to be effective, the new treatment course could improve antibiotic compliance, reduce the development of antibiotic-resistant UTIs, make treatment easier for owners, and save money on prescription costs. UTIs are commonly seen in dogs, especially in females.
Levy CIMAR Scientists Use Artificial Intelligence to Improve Tuberculosis Treatments
Imagine you have 20 new compounds that have shown some effectiveness in treating a disease like tuberculosis (TB), which affects 10 million people worldwide and kills 1.5 million each year. You know that to treat the disease effectively, patients will need a combination of three or four drugs because TB bacteria behave differently in different environments—and in some cases, evolve to become drug-resistant. How do you decide which drugs to test together? Twenty compounds in three- and four-drug combinations offer nearly 6,000 possible combinations.
How the Covid-19 Pandemic Changed Americans’ Health for the Worse
The ripple effects of the Covid-19 pandemic’s influence on nearly every aspect of health in America are becoming clear. Covid-19 has killed more than one million people in the U.S., a toll mounting by some 350 people a day. A range of other chronic diseases and acute threats to health also worsened during the pandemic, data show, as people missed screenings, abandoned routines and experienced loss and isolation. Per the Levy CIMAR’s own Helen Boucher, MD, Dean ad Interim of the Tufts University School of Medicine, antibiotics, strained resources, and a slip in prevention efforts have led to a rise in resistant infections. Experts say that heart disease and drug overdoses are also among afflictions exacting a higher toll than before.
Tufts Announces Springboard Funding Awards to Levy CIMAR Members, Others
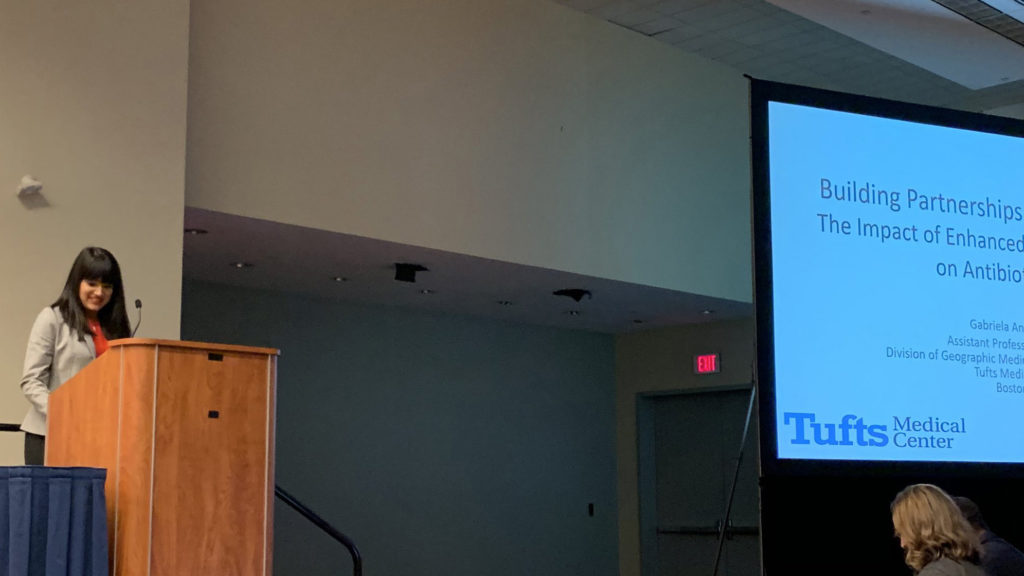
The Tufts University Springboard Award, sponsored by by the Office of the Provost, Office of the Vice Provost for Research (OVPR), and Tufts Medical Center, has a new round of winners. Per the Springboard team, “Each of these high-quality, high-impact research, scholarship, and educational initiatives bodes well for vibrant research at Tufts by having an explicit plan leading to extramural funding or other outcomes that further influence research, scholarship, and/or policy.” Congratulations to all of the winners, and especially to the Levy CIMAR’s own Drs. Alysse Wurcel (TMC), Gabriela Andujar-Vazquez (TMC), Maureen Campion (TMC), Shira Doron (TMC), and Elena Naumova (Friedman), and their colleagues for their important work. Dr. Wurcel and team have been awarded the Springboard prize for their project on “Engaging Stakeholders in New England to Improve Antibiotic Stewardship Practices in Jails and Prisons.” Dr. Naumova and colleagues won the award for their work on “Famine Archive and Data Hackathons.”
Antibiotic-Resistant Infections Could Dwarf the COVID-19 Pandemic
For decades, Boston has been at the forefront of addressing this crisis, from detecting the first MRSA outbreak to the pioneering work of Tufts University’s Stuart Levy, who showed that giving antibiotics to farm animals fuels resistance and threatens human health. Now the city is leading in another critical way: by serving as the global hub of antibiotic financing. Last week the Centers for Disease Control and Prevention announced that US deaths from antibiotic-resistant infections jumped 15 percent in 2020, after years of steady declines. That follows a study published earlier this year in The Lancet that showed 1.27 million people died globally in 2019 from antibiotic-resistant infections, nearly double the number of deaths caused by HIV/AIDS or malaria.
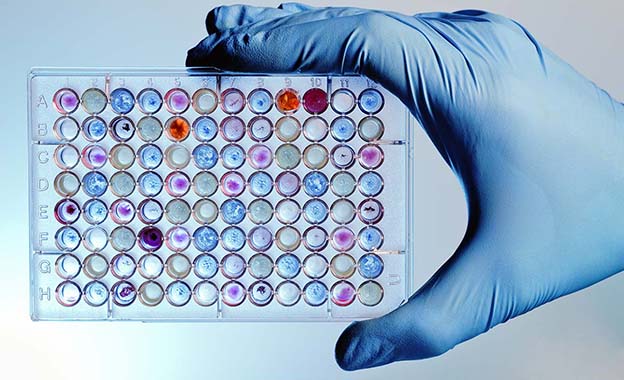
The Levy CIMAR's Dr. Bree Aldridge Explains Combination Drug Therapies, DiaMOND, and How Researchers are Working to Improve Patient Outcomes
Using two or more drugs together as treatment is a simple idea with a complicated underpinning. In order to combine drugs to treat complex infections such as tuberculosis, HIV, and most cancers, we have to understand how their mechanisms work together first. One drug may target one pathway, another drug another pathway. If infected cells grow at different rates, some classes of antibiotics kill the fast-growing cells better, while others are better at killing the slow ones. There can be thousands of combinations to measure. If the right combinations are found, such multidrug therapy may increase treatment efficacy and prevent the development of drug resistance, both important long-term goals.
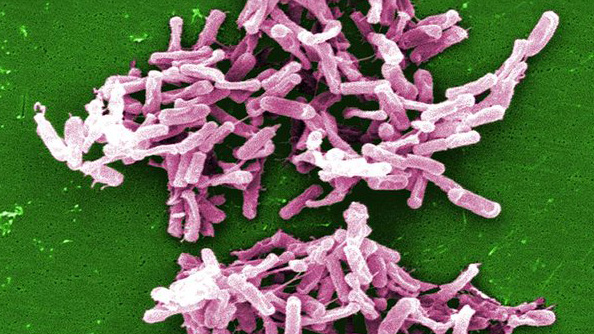
Antibiotic Choices for Skin, Soft Tissue Infections Vary by Race
The Levy CIMAR’s Alysse G. Wurcel, M.D., from Tufts Medical Center in Boston, and colleagues assessed disparities in SSTI treatment using data from the national survey of Acute Care Hospital Groups within Vizient Inc. (Oct.16, 2018, to Jan. 13, 2019). The researchers found that Cefazolin was more commonly used in White inpatients versus Black inpatients (13 versus 5 percent), while clindamycin was more frequently used in Black inpatients than White inpatients (12 versus 7 percent). Cefazolin is one of the first-line SSTI treatments. Clindamycin is not recommended given frequent dosing and high potential for adverse effects including Clostridioides difficile infection.
The Breakthrough Problem, or Why the Drugs Don’t Work Like They Used To
The discovery of drugs appears to obey a rule christened Eroom’s Law. In a nutshell, the number of drugs approved for every billion dollars’ worth of research and development (R&D) halves every nine years. This pattern has remained largely consistent for over 70 years. Since 1950, the cost of developing a new drug has risen at least 80-fold. A Tufts University study suggests that the cost of developing a drug approved by the U.S. Food and Drug Administration (FDA) rose at least 13 times between 1975 and 2009. By the mid-2000s it was $1.3 billion. In the 1960s, by contrast, costs per drug developed were around $5 million. Timelines, at least pre-Covid, are likewise extended. Eroom’s Law shows that it takes more and more effort and money to develop new drugs. Achieving a pharmaceutical breakthrough is on a trend of increasing difficulty.
Boston Doctors Explain How to Time Your Flu, Booster Shots
Drug-Resistant Infections in the US Have Risen Sharply During the Pandemic, and Experts Warn it's Getting Worse as COVID Patients Overwhelm Hospital Resources
Drug-resistant “superbugs” pose a dire threat in hospitals, where an antibiotic-resistant germ like MRSA could leave an already sick patient without any treatment options. Superbugs were a topic of concern in the medical community long before COVID-19 was in our vocabulary, says the Levy CIMAR’s Helen Boucher, MD, an infectious disease physician at Tufts Medical Center and interim dean of Tufts University School of Medicine. “It’s a growing problem, and many of us call it a silent pandemic, because it is, ever, ever so much still with us, despite our very appropriate focus on COVID,” she says.
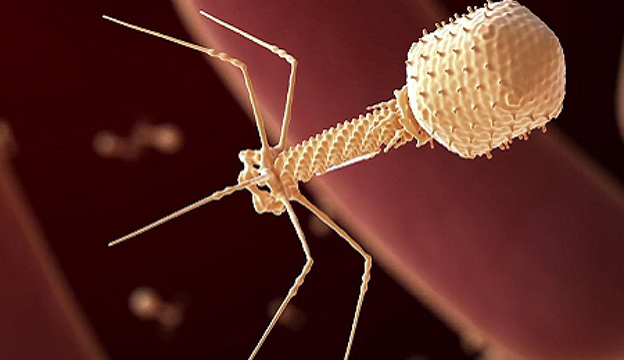
Bacteriophage Therapy Market 2021 Share Leaders, Current Status, Industry Size By Major Key Vendors, Trends
Coherent Market Insights recently published an in depth study of Bacteriophages Therapy Market covering interesting aspects of the market with supporting development scenarios starting from 2021-2027. The report delivers the clean elaborated structure of the Market comprising each and each business-related information of the market at a worldwide level. the entire range of data associated with the worldwide Market is obtained through various sources. PhagePro, Inc., co-founded by the Levy CIMAR’s Andrew Camilli, PhD, is listed among key players focusing on bacteriophage therapies.
Tufts Epidemiologist Breaks Down How New Mask Guidance Applies To Mass.
As COVID-19 cases rise once again, and as variants continue to spread, the Centers for Disease Control and Prevention are recommending that vaccinated people start wearing masks indoors, in many situations. The recommendation applies to areas considered to have a “high and substantial transmission” of COVID-19, and in K-12 schools. The Levy CIMAR’s Dr. Shira Doron, an infectious disease physician and hospital epidemiologist at Tufts Medical Center, joined WBUR’s Morning Edition to discuss what this means for Americanas and how this affects Massachusetts residents in particular.
'Silent Pandemic' Threatens to Turn Back Century of Medical Progress
“Before antibiotics, a simple skin infection had a 10% chance of killing you. People never think about that today, because we have antibiotics that cure all bacterial skin infections. We don’t think about skin infections as being a problem at all,” says Dr. Helen W. Boucher of the Levy CIMAR and interim Dean of the Tufts University School of Medicine in Boston. But now, she warns, time for many of these drugs is running out. Antimicrobial resistance is turning back nearly a century of work to prevent deaths from bacterial and fungal infections. In the U.S. alone, nearly 3 million people annually are believed to fall ill to antibiotic-resistant bacterial infections, and more than 35,000 of the patients die.
A Few Days on Antibiotics Are Often as Good as Weeks, Research Shows
Dozens of studies show that for many bacterial infections, a short course of antibiotics, measured in days, performs as well as the traditional course, measured in weeks. Shorter courses also carry a lower risk of side effects. In April the strength of this research persuaded the American College of Physicians to issue new “best practice advice” for four kinds of infections: pneumonia (the kind acquired in the community rather than in a hospital), “uncomplicated” urinary tract infections (UTIs), skin infections known as cellulitis (provided there is no pus) and acute bronchitis in people with chronic obstructive pulmonary disease.
Concerned About the Delta Variant? This Sports Analogy Helps Explain the Risk
Many people are worried that the rise of the delta variant of the coronavirus, which is more contagious than the earlier variants and has become the dominant strain in the U.S., as well as in Massachusetts. Among the questions people have been wondering is whether they need to wear masks inside again indoors, even if they’ve been vaccinated. The World Health Organization recently said they should, but the U.S. Centers for Disease Control and Prevention says that’s unnecessary.Experts including the Levy CIMAR’s Dr. Shira Doron, an infectious disease physician and epidemiologist at Tufts Medical Center, weigh in.
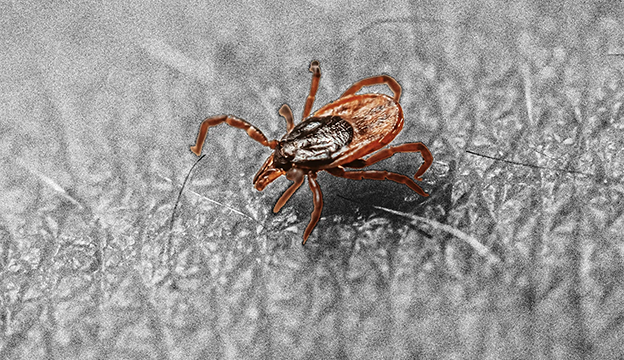
There’s a Vaccine for Lyme Disease. So Why Can’t We Get It?
Thanks to vaccines, the number of COVID-19 cases has plummeted in the U.S. and restrictions are being lifted across the country. But as we return to our normal activities, we face a more familiar summertime scourge. We’re in the thick of Lyme disease season, the two-month run from early June to the end of July when 85 percent of infections take place. Surprisingly, vaccines may have allowed us to avoid this epidemic, too. A vaccine called LYMErix has existed for decades, but it’s no longer available. In this article, you will learn why LYMErix is no longer available and discover where the research stands today.
Helen Boucher Named Interim Dean at Tufts University School of Medicine
Helen Boucher, MD, chief of the Division of Geographic Medicine and Infectious Diseases at Tufts Medical Center, professor of medicine at Tufts University School of Medicine, and a director of the Stuart B. Levy Center for Integrated Management of Antimicrobial Resistance (Levy CIMAR), has been named to a new, joint position as interim dean for Tufts University School of Medicine and chief academic officer for Wellforce, beginning July 1. Dr. Boucher will be the first woman to lead the School of Medicine in its 128-year history. Cheleste Thorpe, MD, will step in as Interim Director to lead the Levy CIMAR alongside Director Ralph Isberg, PhD.
Plotting the End of Lyme Disease: Tufts Researchers Lead the Cutting Edge of Fighting this Mysterious Illness
As people weary of being cooped up during a pandemic winter look forward to a summer outside, residents across the northeastern United States are once again confronted with a familiar virulent pathogen lurking in the woods and fields. Unlike coronavirus, however, this dangerous microorganism doesn’t float through the air—it enters the body through the bite of a tick. Lyme disease has been a constant scourge since it was identified five decades ago on the Connecticut coastline, before spreading across the New England and Mid-Atlantic states. Several Levy CIMAR are involved in the fight against Lyme including Senior Leadership Members Drs. David Snydman and John Leong.
2021 Sanctae Crucis Recipients Honored for Leadership During Pandemic
Last week, the College of the Holy Cross presented seven alumni with Sanctae Crucis Awards for their extraordinary commitment and leadership in critical fields throughout the COVID-19 pandemic. The Sanctae Crucis Award is the highest non-degree accolade that the College bestows on alumni. The awards have been presented annually since 1998 to alumni who have distinguished themselves professionally and in the service of their community. Among the awardees is Levy CIMAR Director Dr. Helen Boucher, Chief of Infectious Diseases at Tufts Medical Center. She graduated from Holy Cross in 1986 prior to attending the University of Texas Medical School in Houston.
Antibiotic Development, Stewardship Advocates See Window of Opportunity
The pandemic isn’t over yet, but with more and more Americans getting vaccinated against COVID-19 and the light at the end of the pandemic tunnel becoming a little brighter every day—at least in the United States—many clinicians, scientists, and public health advocates are calling for renewed attention to an infectious disease threat that was in the spotlight before the pandemic arrived. Prior to the pandemic, antimicrobial resistance (AMR) was considered one of the major looming health threats facing the world, if not the looming threat. But over the past year, COVID-19, and its multifaceted impact on society, has pushed AMR further back on the agenda, both for the public and policy makers.
Preventing the Next Public Health Crisis of AMR Can Define Biden's Legacy
In this guest column, Levy CIMAR Director Dr. Helen Boucher says, “The Biden administration’s plan to defeat the coronavirus is underway – and notably includes intentions to ‘build better preparedness for future threats.’ This detailed guidance could not have come at a better time. While we are making progress against the current pandemic, we remain in the midst of a worsening health crisis posed by antibiotic resistance. Deadly bacteria, commonly known as ‘superbugs,’ are evolving to resist even our strongest antibiotics, and we’re not even close to developing enough new treatments to keep pace.”
Doctors' Group Says Antibiotics Can Be Taken for Shorter Periods
Millions of Americans have at some point in their lives gotten a long course of antibiotics to treat a bacterial infection. But according to new recommendations from a major U.S. doctors’ group, some of the most common bacterial infections can now be treated with shorter courses of the drugs. The advice, from the American College of Physicians (ACP), says that for several types of infections, shorter courses of antibiotics do the job — and even do it more safely. “Antibiotics can be lifesaving, but like any medication, they have side effects,” says Levy CIMAR Director Dr. Helen Boucher.
NIH Awards Grants to Support Bacteriophage Therapy Research
The NIH has awarded $2.5 million in grants to 12 institutes around the world to support research on bacteriophage therapy. Boston-based PhagePro, Inc. and Principal Investigators Minmin Yen and the Levy CIMAR’s Andrew Camilli were among the recipients named. These awards represent NIAID’s first series of grants focused exclusively on research on this therapy, an emerging field that could yield new ways to fight antimicrobial-resistant bacteria. A 2019 report from CDC found that antibiotic-resistant pathogens cause more than 2.8 million infections in the U.S. each year and more than 35,000 people die.
Levy CIMAR Joins Forces with Filmmakers for 'Beating Superbugs' Documentary and Panel World Premiere
“The pandemic has forced keen awareness of a topic that most people would rather not talk about,” says Beating Superbugs: How Can We Win? filmmaker Bill Mudge. “Most importantly, we emphasize real solutions rather than feeding an all too pervasive crisis fatigue. Regardless, there’s nothing quick, cheap, or easy about containing superbugs but it definitely can be done.” You can now watch this timely film and panel event, featuring several experts including our own Dr. Helen Boucher, as well asa our affiliate member Dr. Muhammad Zaman, from your mobile devices, computers, or TVs on Vimeo.
Tufts Medical Center Begins Administering Johnson & Johnson COVID-19 Vaccine
Tufts Medical Center in Boston began administering the Johnson & Johnson COVID-19 vaccine Thursday, giving Massachusetts a third vaccination option in its push to get more shots in arms. The Levy CIMAR’s Helen Boucher, Chief of Infectious Diseases at Tufts Medical Center, urged vaccinated residents to continue to keep their guard up to protect themselves and others.“I encourage people as good citizens and good Americans to continue to wear their masks,” she said. Watch the full story on WHDH online.
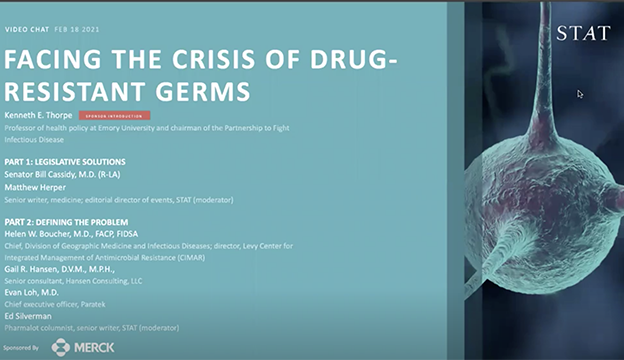
Facing the Crisis of Drug-Resistant Germs: An Expert Panel Hosted by STAT News
The COVID-19 pandemic has shown what happens when we let our guard down against infectious disease, despite years of increasingly loud warnings. So it’s time to be even more worried about antibiotic-resistant germs. What policy steps can fight this growing problem? Recently STAT convened policymakers, researchers, and corporate executives to chart a path to progress. Levy CIMAR Director Helen W. Boucher M.D., Chief of Division of Geographic Medicine and Infectious Diseases at Tufts Medical Center, joined the discussion.
Antibiotic Resistance: A Call to Action to Prevent the Next Epidemic of Inequality
The COVID-19 pandemic has revealed the deadly impacts of structural racism and systemic health inequalities on racial and ethnic minorities in the USA. Black and Hispanic/Latinx populations have been disproportionately impacted by COVID-19, accounting for nearly half of the cases and 37% of the deaths so far, despite making up less than a third of the US population. This stark imbalance has highlighted the need to examine the role of racial and ethnic disparities in shaping health outcomes, particularly with respect to Antimicrobial Resistance, say Levy CIMAR’s Drs. Maya Nadimpalli and Shira Doron.
With Ticks Spreading Across the Country, the CDC Says There May Be Nearly Half a Million Cases of Lyme Annually
Between 2010 and 2018, the U.S. had approximately 476,000 cases of Lyme disease every year, according to the CDC. That number is substantially higher than the CDC’s previous estimates, of about 300,000 annual Lyme cases. Linden Hu, MD, of the Tufts Lyme Disease Initiative, notes that the true number of cases of Lyme disease probably varies widely from one year to the next based on changes in tick density in different areas, weather patterns, and more. Still, he says, “there certainly are a lot of cases, and based on the spread of tick range, and things like that, we do anticipate that there’s an upward trend.”
Levy CIMAR's Amy Pickering Joins Berkeley Faculty
Amy Pickering, PhD, has joined the faculty at UC Berkeley as Assistant Professor in Development Engineering, a joint Blum Center-College of Engineering appointment made possible through a generous gift from Richard C. Blum and an anonymous donor. There, she is also the Blum Center Distinguished Chair in Global Poverty and Practice. Pickering, formerly a Tiampo Family Assistant Professor in Civil and Environmental Engineering at Tufts University and a distinguished member of the Levy CIMAR, is now a Levy CIMAR Affiliate Member as of January 2021.
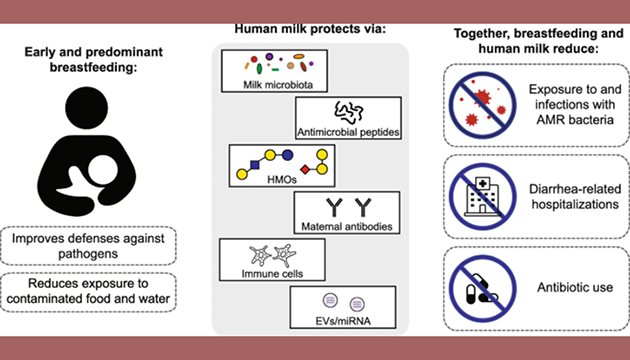
Opinion: Can Breastfeeding Protect Against Antimicrobial Resistance?
The proportion of infections among young children that are antimicrobial-resistant is increasing across the globe. Newborns may be colonized with enteric antimicrobial-resistant pathogens early in life, which is a risk factor for infection-related morbidity and mortality. Levy CIMAR Core Faculty Members, Maya Nadimpalli, PhD, Amy Pickering, PhD, and colleagues say that breastfeeding and human milk supplements deserve greater attention as potential preventive measures in the global effort to combat AMR, particularly in low- and middle-income settings. Recent evidence supports the role of breastfeeding in preventing the acquisition, establishment, and proliferation of enteric pathogens, including AMR bacteria.
Opinion: To Defeat COVID-19, We Must Acknowledge the Fear it Engenders
“My career as a hospital epidemiologist has been based on science and evidence, which I believed to be the touchstones of my work,” says Levy CIMAR Core Faculty member Shira Doron, MD. “But COVID-19 has taught me that fear — gut-wrenching, all-consuming fear, like the fear of dying from a horrific respiratory virus — can be much more powerful than science. We can’t conquer this fear unless we acknowledge and respect it. I’m no stranger to my work keeping me awake at night. In pre-pandemic times, I sometimes lost sleep over issues like a spike in staph infections in a particular intensive care unit. Now I lie awake worrying about keeping patients safe from COVID-19.”
Levy CIMAR's Helen Boucher, MD, on SARS-CoV-2 Vaccines
Massachusetts could receive enough doses of Pfizer’s vaccine by Christmas to vaccinate 300,000 people. How significant is that number? And how quickly could it slow our rate of new cases? According to Levy CIMAR Director Helen Boucher, MD, Chief of Infectious Diseases at Tufts Medical Center: “That is a significant number. It is a larger number than we had expected, so this is good news. I do think we have to temper that with understanding it is going to take weeks to months before we reach the levels of immunity that will stop the spread of the virus. I think our estimates of some time to the spring and summer next year before we reach that 60-70% to allow us to get back to everyday activities is still reasonable.”
Webinar: Addressing HIV Drug Resistance to Protect the Effectiveness of HIV Treatment
Over the past decade, the world has witnessed unprecedented scale-up of antiretroviral therapy (ART) which has saved the lives of tens of millions of people. As of December 2019, 25.4 million people out of an estimated 38 million people living with HIV were receiving ART globally. Increased use of ART has, not unexpectedly, been accompanied by the emergence of some degree of HIV drug resistance, the levels of which have steadily increased in recent years. Join the WHO and experts in the field including the Levy CIMAR’s Michael Jordan, MD, for a webinar on “Addressing HIV drug resistance to protect the effectiveness of HIV treatment” in celebration of World Antimicrobial Awareness Week.
Here’s Why a Negative COVID-19 Test Doesn’t Guarantee You Can Safely Gather on Thanksgiving
If you’re planning on relying on a COVID-19 test as the go-ahead before spending Thanksgiving with people from other households, experts say that doesn’t necessarily ensure the virus won’t spread. “A test is just one point in time,” said Levy CIMAR Director Dr. Helen Boucher, chief of infectious diseases at Tufts Medical Center. “The incubation period for this virus is 14 days. Just because someone tests negative today doesn’t mean they won’t be positive tomorrow or in the next 13 days.” A large dinner in which people from different households sit closely together indoors, maskless, could create a “perfect storm” for COVID19 spread, she said.
Experts Warn Antibiotic-Resistant ‘Superbugs’ Could Be Next Public Health Epidemic
The global COVID-19 pandemic has been raging on for months, but some experts warn another health crisis is looming: Antibiotic-resistant bacteria or so-called “superbugs.” Levy CIMAR Director Dr. Helen Boucher said drug-resistant infections have grown significantly in the past 10 years due to antibiotic overuse and misuse. She said some doctors are overprescribing drugs and some patients are not taking them properly. “We shouldn’t ask for antibiotics for things like colds which are caused by viruses and for which antibiotics won’t help,” Boucher said. “We should really take them, these precious medicines, exactly as prescribed so we can do our part to prevent more resistance.”
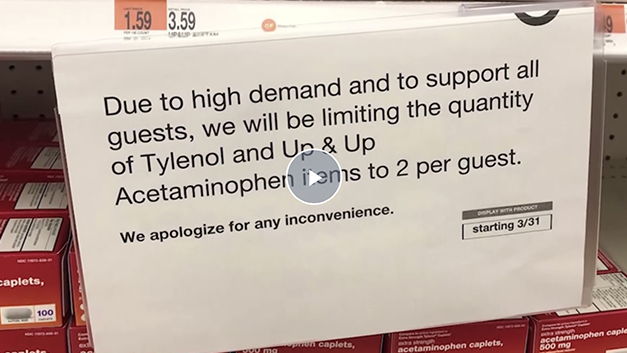
Treating COVID-19 Patients Leads to Short Supply of Certain Common Drugs
According to the Center for Infectious Disease Research and Policy, caring for COVID-19 patients is causing shortages of that drug and several others, including heart medication norepinephrine, albuterol inhalers which are often used by asthma patients, certain antibiotics and propofol, a sedative used to calm patients while they are intubated. “Just like testing materials, medical equipment and PPE, drugs — even the ones we commonly use for everyday medical conditions and hospitalized patients — are in short supply since the pandemic began, and all of those shortages have the potential to negatively impact the care of patients in Boston,” said Levy CIMAR’s Dr. Shira Doron, an epidemiologist with Tufts Medical Center.
Levy CIMAR's Shira Doron on Why Rising COVID-19 Levels in Wastewater is Concerning
Tufts Medical Center Hospital Epidemiologist and Levy CIMAR Core Faculty Member Dr. Shira Doron discusses the increase in COVID-19 cases in Massachusetts, the role of social gatherings in spreading the virus, coronavirus in wastewater, and shortages of critical drugs in her weekly appearance on WCVB. ‘The data suggests that right now, every infected person is on average transmitting the infection to more than one other person,” says Doron. ” Therefore, if we change nothing at all, we can expect to see the numbers continue to rise faster and faster. The time is now to double down on those efforts to avoid situations.”
How Researchers are Revamping Antimicrobial Drugs
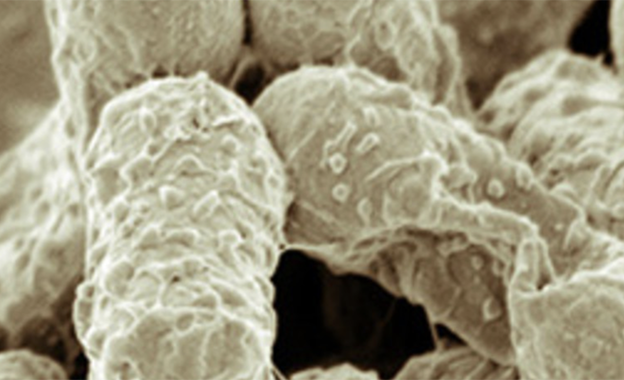
There’s a long road from discovering a potential drug to getting it approved for human use. Levy CIMAR’s Bree Aldridge, Ph.D., thinks the process could be speeded up by using a computerized imaging system that looks at how bacterial cells are deformed by a drug. Such changes can give hints as to what part of a cell’s biology the drug is acting on. “We think we know what a drug does, but then if you look at how it actually destroys the cells, we can sometimes see that it’s a little bit different,” Aldridge says. “This sort of method allows us to rapidly determine whether a drug is acting like known drugs or whether a drug is doing something that’s novel.” If it’s novel, it might be a class that bacteria are not yet resistant to.
U.S. Updates Antibiotic Resistance Plan: Here's What's New
The U.S. government released an update to its National Action Plan for Combating Antibiotic-Resistant Bacteria (NAP CARB), which aims to combat antibiotic-resistant bacteria and subsequent infections. There are more than 2.8 million antibiotic-resistant infections—and 35,000 deaths—in the U.S. each year. Among other things, the Plan aims to slow the growth of resistant bacteria and prevent infections from spreading, strengthen surveillance efforts, and advance development and use of rapid diagnostic tests.
A Call for Global Monitoring of WASH in Wet Markets
“Regardless of the role wet markets will play in future respiratory virus epidemics, wet markets pose additional zoonotic health risks that must be prioritised by global health researchers and policy makers. Specifically, wet markets could be hotspots for enteric pathogen transmission because of poor and unregulated hygiene conditions. … Building improved wet market infrastructure is urgently needed, particularly in low-resource settings.” — Levy CIMAR Core Faculty members Drs. Maya Nadimpalli and Amy Pickering
Center for Antimicrobial Resistance Renamed for Stuart B. Levy
The Center for Integrated Management of Antimicrobial Resistance, a collaborative effort supported by Tufts University and Tufts Medical Center, has been renamed the Stuart B. Levy Center for Integrated Management of Antimicrobial Resistance (Levy CIMAR) at Tufts, in honor of the pioneering antibiotic-resistance researcher. Levy, a professor emeritus of molecular biology and microbiology at Tufts University School of Medicine and a staff physician at Tufts Medical Center, passed away in September 2019 at the age of 80. He retired in 2018 after 47 years at Tufts.
As a Virus Ravages the World, Antibiotic Makers are in Disarray
COVID-19 can be accompanied by secondary bacterial infections with deadly consequences. But the industry that researches and produces antibiotics to fight such illnesses has been upended — and the pandemic is only making things worse. Now, medical experts worry about the long-term health implications of not having cutting-edge antibiotics in the pharmaceutical pipeline. Per CIMAR Dir. Dr. Helen Boucher: “This need to have a robust and renewable pipeline of antibiotics has really never been greater.
IDSA, APHA Call on White House to Reverse Handling of COVID-19 Data
A letter sent by the leadership of the Infectious Disease Society of America (IDSA) including board member, CIMAR Dir. Dr. Helen Boucher, as well as those from dozens of other organizations calls on the Trump administration to reverse its decision to bypass the US Centers for Disease Control and Prevention (CDC) in “the collection and analysis of COVID-19 patient data.”
New Cell Profiling Method Could Speed TB Drug Discovery
A new technology that combines high throughput imaging and machine learning could speed discovery of drugs to fight tuberculosis, which for generations has killed more people worldwide than any other disease caused by a single agent—4,000 people every day. “We urgently need shorter, more effective TB therapies, and MorphEUS enables us to screen through drug candidates, see how they actually affect the cell, and learn which drugs have unique ways to kill the M. tb,” says CIMAR’s Dr.Bree Aldridge.
Dr. Helen Boucher Discusses The COVID19 Infection Curve, What To Expect In Mass.
Nearly 20,000 people have now tested positive for the novel coronavirus in Massachusetts. Well over 500 have died. With the surge in COVID-19 hospitalizations fast approaching in Massachusetts, WBUR’s Weekend Edition joined Dr. Helen Boucher, chief of the Division of Geographic Medicine and Infectious Diseases at Tufts Medical Center, to discuss where we are now on the infection curve and what to expect in the coming weeks.
CIMAR and Tufts Medical Center's Dr. Shira Doron Discusses What SARS-CoV2 Antibody Tests Might Reveal
Dr. Shira Doron, Core Faculty Member of CIMAR and hospital epidemiologist at Tufts Medical Center, answers questions about what the hospital is seeing in patients and what antibody tests available may show. She also discusses the anticipated surge in COVID-19 hospitalizations in Massachusetts and more.
CIMAR's Dr. Helen Boucher: "Have We Made Progress in the 10 X' 20 Initative?"
Antibiotics make procedures including joint replacement, transplantation, cancer chemotherapy, and premature newborn care possible. Recent reports have warned of the dangerously failing antibiotic pipeline; on January 18, the World Health Organization issued an unprecedented warning, declaring that “only government intervention can fix the broken market for antimicrobial drugs.”
3 Surprising Traits of How COVID-19 Affects Patients According to Experts
One surprising trait: Patients who seem to be recovering can suddenly crash. CIMAR’s Dr. Gabriela Andujar Vazquez, an infectious disease physician at Tufts Medical Center in Boston, said patients should also watch for chest pain, and advised anyone experiencing chest pain or breathing difficulty to head to the emergency room. “People need to really monitor themselves for the first week. After the first week, you’ll either get better or worse,” she says.
How Long Does Coronavirus Live On Clothes? Doctors Weigh In
Most of the time, we can count on our clothes to offer us protection from the outside world. In the midst of the novel coronavirus pandemic, however, it’s easy to see them as a potential threat — particularly if you’re not sure how you should be washing them. If you’ve arrived home from errands concerned about how long coronavirus live on your clothes, it may offer comfort that by staying vigilant, you can safely re-wear favorite pieces and dress how you please.
Calculations, Concerns, & Crisis: The struggle to find masks and gowns spurs local hospitals to make drastic decisions
CIMAR’s Dr. Shira Doron, an infectious disease physician and epidemiologist at Tufts Medical Center, was exhausted. Minute by minute, the supply numbers changed, donations came in, patient predictions soared. At this rate, if patient numbers doubled daily, staff would run out of masks in a matter of days. If the health system could go through fewer supplies each day, a slower burn rate, maybe they could last a few weeks.
Tufts Medical Chief of Infectious Diseases Discusses What Doctors are Doing to Fight COVID-19
CIMAR Director Dr. Helen Boucher discusses the training that goes into being an infectious diseases specialist, as well as what ID clinicians such as herself are doing to diagnose, treat, educate, and protect the public in the face of the COVID-19 pandemic.
"Continue What We’re Doing as Long as Possible:" CIMAR's Dr. Shira Doron Says Social Distancing Must Continue
While some politicians, including the President, are looking to ease restrictions keeping people from work, CIMAR’s Dr. Shira Doron (an Attending Physician, Hospital Epidemiologist, and Antimicrobial Steward at Tufts Medical Center) says distancing needs to continue during the COVID-19 pandemic while medical professionals deal with a shortage of supplies.
Food Delivery Safety During the Coronavirus Pandemic: What You Need to Know
CIMAR featured trainee, Dr. Gabriela Andujar Vazquez, has several tips including calling up any restaurant you plan on ordering from and asking specific questions about what they’re doing to deter the spread of coronavirus at all stages of the cooking and handling process.
Health Expert Urges Parents to Minimize Play Dates Amid Coronavirus Fears
With schools shut down across the Bay State for the next three weeks in an attempt to stop the spread of the coronavirus, parents are faced with the tough question of whether or not to let their kids socialize. CIMAR’s Dr. Helen Boucher is urging families to think small when it comes to playdates.
More Of Your Questions About The Coronavirus, Answered
CIMAR Director Dr. Helen Boucher, Chief of Geographic Medicine and Infectious Diseases at Tufts Medical Center, and Dr. Joshua Barocas of Boston Medical Center and the Boston University School of Medicine joined WBUR to answer listener questions about COVID-19/Novel Coronavirus.
Coronavirus Cases Are On The Rise In New England
The number of coronavirus cases in Massachusetts is climbing. CIMAR Director Dr. Helen Boucher, Chief of Geographic Medicines and Infectious Disease at Tufts Medical Center, joined WBUR’s Morning Edition host Bob Oakes to help put the numbers in perspective.
W.H.O. Warns That Pipeline for New Antibiotics Is Running Dry
In two new reports, the global health agency says only government intervention can fix the broken market for new antimicrobial drugs. “We can’t have more companies going bankrupt,” said CIMAR Director Dr. Helen Boucher, an infectious disease specialist at Tufts Medical Center and a member of the Presidential Advisory Council on Combating Antibiotic-Resistant Bacteria. “If the pipeline remains this anemic, that’s going to have real implications for our patients.”
Heroic Motorized Molecules Drill Superbug Full of Holes
All manner of fancy ideas have been floated to kill the superbug, when what we’ve needed is a hero willing to go toe-to-toe with these pitiless, heavily-armored bacteria. And here it is: a seek-and-destroy motorized molecular drill that is activated by light to “spin at three million rotations per second” – and ruthlessly disembowel the enemy outright. Notably, the world’s first single molecule electric motor was developed at Tufts University’s School of Arts and Sciences in 2011.
Antibiotic Makers Struggle, Hurting War on Superbugs
One of America’s biggest antibiotics specialists, Melinta Therapeutics Inc., filed for bankruptcy in late December, citing slow sales growth and high costs. Other makers might soon face a similar fate, saying their cash will run out before the end of 2020. “We don’t know the fate of those drugs for our patients,” said CIMAR Director Helen Boucher, chief of infectious diseases at Tufts Medical Center in Boston. “As a physician, that’s my biggest concern.”
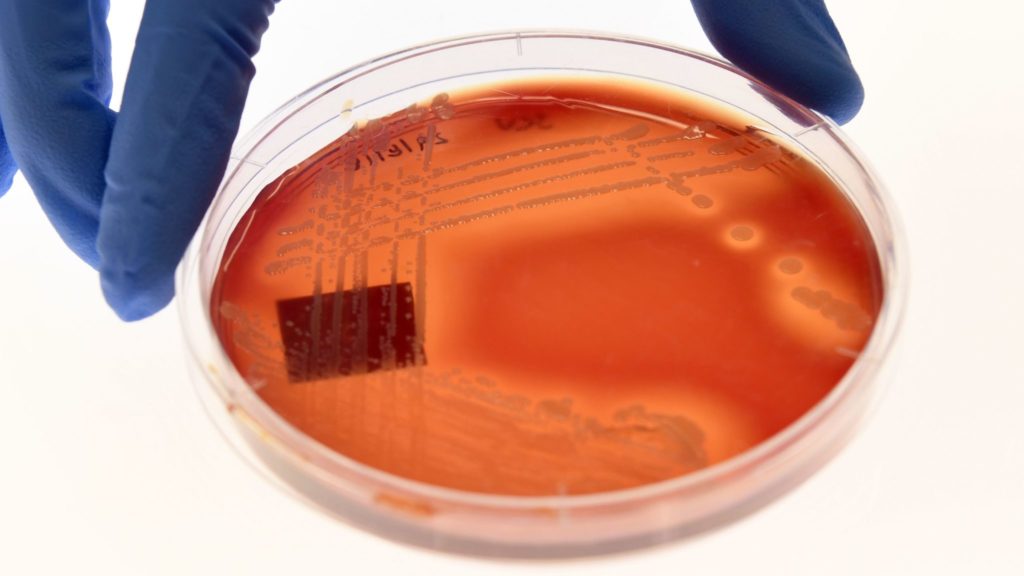
Deadly Superbugs Pose Greater Threat Than Previously Estimated
Drug-resistant germs sicken about 3 million people every year in the United States and kill about 35,000, representing a much larger public health threat than previously understood, according to a long-awaited report released Wednesday by the Centers for Disease Control and Prevention. The new estimates show that, on average, someone in the United States gets an antibiotic-resistant infection every 11 seconds, and every 15 minutes, someone dies.
‘Superbug’ Infections are on the Rise, a New CDC Report Says
“We see people from everyday life, who are young and otherwise healthy, who get a MRSA [methicillin-resistant Staphylococcus aureus] infection on their skin,” says CIMAR Director Dr. Helen Boucher. “We want to have diagnostic tools and medical treatments for problems we know we’re going to have,” she said. “But we also need to prepare for the kind of resistance that we could never predict. We know from history that bacteria and mother nature are smarter than we are.”
New Antibiotics Needed "Yesterday" to Tackle Drug-Resistant Infections, Says CIMAR Director
When Roxana Sudderth’s son, Trey, a healthy high school freshman, developed a sore on his foot after playing basketball, “it just looked like a small blister.” Doctors gave him antibiotics, but the pain persisted. Sudderth took him to the hospital where they told her he had a life-threatening infection, MRSA, a bacterium resistant to antibiotics. Over 19 days, his condition deteriorated until finally doctors told Sudderth it was time to take Trey off life support.
Unlocking Biological Materials for Better Therapies
Researchers at Tufts’ Laboratory for Living Devices (L2D) link materials like silk and paper with technology, medicine, and diagnostics. CIMAR and L2D faculty member, Dr. Bree Aldridge, and her team are using biomaterials made of silk to engineer programmable diagnostic platforms—or “petri dishes of the future”—to fight antimicrobial resistance by gathering more detailed information about susceptibility to multiple drugs.
Wellcome Trust Report Urges Better Antimicrobial Resistance Messaging
A new report suggests clinicians, public health professionals, and journalists need to rethink the way they talk about antimicrobial resistance to increase public understanding and promote action by policy makers. In this article, CIMAR Director Dr. Helen Boucher acknowledges that while it is challenging issue to explain to the public, stakeholders haven’t done a great job of communicating the immediacy and severity of antimicrobial resistance.
Is the Gene-Editing Tool, Crispr, the Next Antibiotic?
Desperate to find new medicines against pathogenic microorganisms, scientists are turning to Crispr, which has typically been considered for macroscopic tasks: altering mosquitoes so they can’t spread malaria, editing tomatoes so they are more flavorful and curing certain genetic diseases in humans. Now researchers are harnessing Crispr to turn a bacterium’s machinery against itself, or against viruses that infect human cells.
CIMAR LEAP Fellow Presents Groundbreaking Antimicrobial Stewardship Findings at IDWeek
Dr. Gabriela Andujar Vazquez presented groundbreaking findings from her antimicrobial stewardship pilot study at IDWeek in Washington, D.C. earlier this month. The study showed a 20% decrease in antibiotic start rate in patients, potentially demonstrating the benefit of enhanced stewardship support by an expert on antibiotic use in long term care.
Antibiotics Are Losing Their Power Against Deadly Infections. Can We Fix the Problem?
Experts say the problem of AMR is compounded by improper use of antibiotics by doctors, hospitals and patients, as well as by farmers and others in the agricultural sector (the drugs are commonly administered to livestock, as well as to humans). Check out this eye-opening panel discussion from CIMAR’s Dr. Helen Boucher and others.
ASM Podcast Honors the Life and Legacy of Dr. Stuart Levy
The TWiM holobionts pay tribute to Stuart Levy, and reveal the remarkably diverse array of cyclic nucleotides synthesized by bacteria that likely mediate interactions with animal and plant hosts. Dr. Levy’s friends and colleagues, Drs. Elio Schaechter and Michele Swanson, join the discussion.
Remembering Stuart Levy, a Pioneer Who Sounded the Alarm on the Threat of Antimicrobial Resistance
Stuart B. Levy, a key inspiration for CIMAR and an Emeritus Professor of Molecular Biology and Microbiology at the Tufts University School of Medicine, died following an extended illness on September 4th. Dr. Levy’s pioneering research and impassioned advocacy raised awareness of the danger of antibiotic resistance, He was 80. Colleagues, friends and family remember Dr. Levy in this piece from TuftsNow.
Why is there an EEE Vaccine for Horses but not for Humans?
Actually, there is a human vaccine for eastern equine encephalitis (EEE), but it has never been approved for public use. The U.S. Army Medical Research Institute of Infectious Diseases—the military medical research institute at Fort Detrick in Maryland—developed a human EEE vaccine in the mid-1980s. Tufts Cummings School Professor Sam Telford, an expert on infections spread by mosquitoes and ticks, explains.
Tufts Cummings Vet School Hosts Symposium on "Engaging Veterinarians to Advance Human and Animal Health"
Nearly 600 veterinary students from the U.S., Canada, and beyond attended the 30th National Veterinary Scholars Symposium, hosted by the Cummings School of Veterinary Medicine at Tufts University. The meeting featured topics on critical care, antimicrobial resistance, regenerative medicine, cancer biology, infectious diseases, and pathways to research career development.
New Antibiotic Approved for Drug-Resistant Tuberculosis
The Food and Drug Administration has approved a new drug for highly drug-resistant tuberculosis, the world’s leading infectious cause of death. The antibiotic, called pretomanid, was developed by a nonprofit group called TB Alliance at a time when few companies are investing in the expensive and unprofitable endeavor of creating next-generation antibiotics. CIMAR Director Dr. Helen Boucher shares her insights.
Tufts Researchers Focus on Mice as Potential Solution to Lyme Disease
New England has some of the highest rates of Lyme disease in the country. In 2017, there were more than 400 confirmed and probable cases in Massachusetts. In Maine, the number of confirmed and probable cases was more than 1,800. Now, a unique project aims to stop the disease in its tracks by going straight to the source.
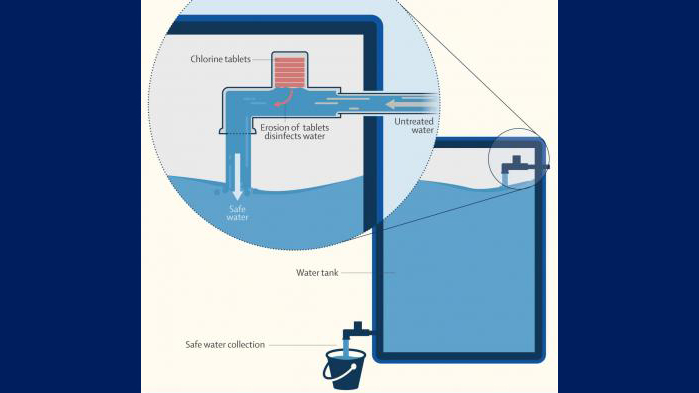
Automatically Chlorinating Water Reduces Diarrheal Diseases in Children in Urban Bangladesh
“This novel, low-cost technology requires no behavior change or effort by users–safe water comes straight out of the tap,” says CIMAR’s Dr Amy Pickering, who led the research. “This point-of-collection approach to water treatment could be a transformative strategy for reducing gastrointestinal disease burden in low-income urban communities.”
Overdue Outbreak Detection System Leaves Patchwork Defense
According to CIMAR Director Dr. Helen Boucher and others, the U.S. should have had a nationwide network to monitor for the next viral outbreak or biological threat a decade ago. Instead, public health leaders make do with a patchwork system while waiting for the Department of Health and Human Services races to get its integrated network in service.
Call the Bee Vet: Bee Keepers Can No Longer Get Antibiotics Over the Counter
Shortly after the FDA directive mandating that any antibiotics for honeybees be prescribed by veterinarians, Tufts Cummings School offered a sold-out continuing-education bee medicine workshop for practicing veterinarians. Tufts hopes to offer more training for veterinarians in the near future.
Antibiotics Developers Seek a Cure for Industry Ills
Not long ago, Achaogen Inc. was flying high. In early 2017, the drugmaker’s market capitalization soared above $1 billion on high hopes for its new medicine, an antibiotic targeting complicated urinary-tract infections. But in April—less than a year after the drug was approved by the Food and Drug Administration—Achaogen filed for bankruptcy.
IDSA Describes AMR Challenges, Answers in Congressional Testimony
The Infectious Diseases Society of America (IDSA) treasurer Dr. Helen Boucher, FIDSA, has urged lawmakers to support and expand federal efforts to stabilize the antibiotic market, spur the development of new infection-fighting drugs and protect existing ones in testimony before House Oversight and Reform Subcommittee on National Security.
Antibiotic Resistance Plays a Role in Biodefense
The House Oversight subcommittee on national security convened experts last week to discuss biodefense — and the focus was on the threat of antimicrobial resistance. A bug doesn’t have to be a weapon to be deadly. “We have the sad duty of sending people to hospice because we don’t know how to treat their infections,” CIMAR’s Dr. Helen Boucher told the panel.
Experts Warn of Antimicrobial Resistance, Additional Threats to National Biosecurity
“Antibiotic infections pose serious threats to our national security,” said Dr. Helen Boucher, director of the Tufts Center for Integrated Management of Antimicrobial Resistance at Tufts University. “Resistant pathogens complicate our soldiers’ combat wounds, increasing risk of limb loss and death, and compromise our military combat readiness and effectiveness.”
CIMAR Epidemiologist Maya Nadimpalli, PhD, Describes Efforts to Document Antibiotic Resistance in Developing Countries
As an epidemiology postdoc at the Pasteur Institute in Paris, Maya Nadimpalli became interested in antibiotic resistance among young children in low-income countries. Now at Tufts University in Boston, Massachusetts, Nadimpalli shares the opportunities and challenges of studying public health in developing nations in this Nature Careers Q&A.
CIMAR's Yoav Golan, MD, on the Recent Approval of Ceftolozane/Tazobactam for HABP/VABP
The FDA has approved a new indication for Merck’s ceftolozane/tazobactam (Zerbaxa), allowing for the drug to be used to treat hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia. Contagion® spoke with CIMAR’s Yoav Golan, MD, attending physician and associate professor of medicine at Tufts University School of Medicine, about what this could mean for patients.
Phage Therapy to Prevent Cholera Infections--and Possibly Those Caused by Other Deadly Bacteria
In the latest of a string of high-profile cases in the U.S., a cocktail of bacteria-killing viruses successfully treated a cystic fibrosis patient suffering from a deadly infection caused by a pathogen that was resistant to multiple forms of antibiotics. Curing infections is great, of course. But what about using these bacteria-killing viruses to prevent infections in the first place?
Joining Forces for Good: Tufts CIMAR and the Tufts Clinical and Translational Science Institute Encourage Multidisciplinary Collaboration.
CIMAR and CTSI are just two of the exciting initiatives that embody Tufts’ commitment to enhancing multi-disciplinary collaboration. Each brings together investigators and clinicians from across the medical school, the university, and Tufts Medical Center to solve pressing real-world problems with a One Health approach.
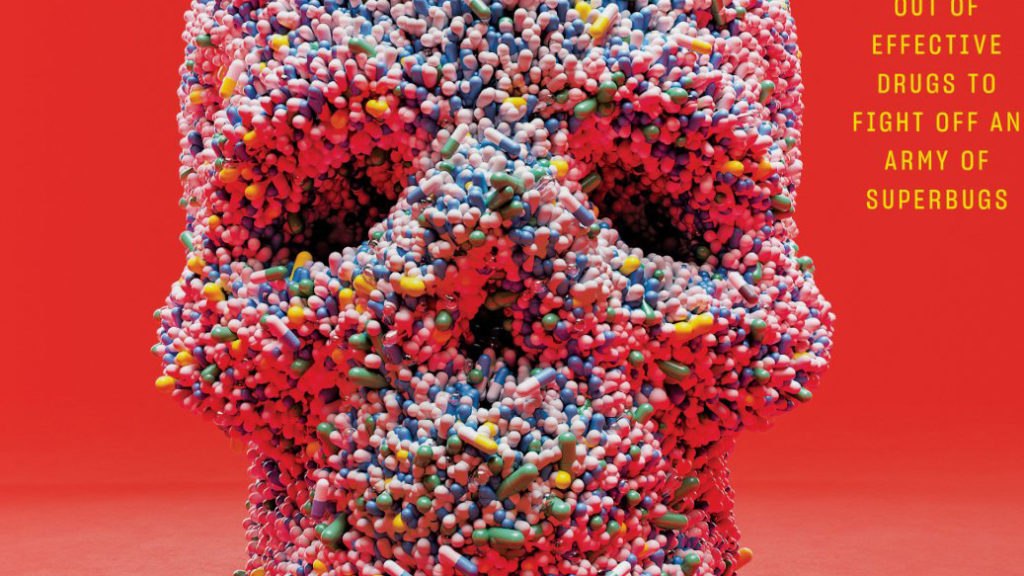
The Death of Antibiotics: We’re Running Out of Effective Drugs to Fight Off an Army of Superbugs
“We’re seeing healthy young people with urinary tract and skin infections that we don’t have a pill for,” says Helen Boucher, an infectious disease specialist at Tufts Medical Center in Boston. “And we may not be able to perform organ transplants, and even routine surgeries like joint replacements. We should all be scared.”
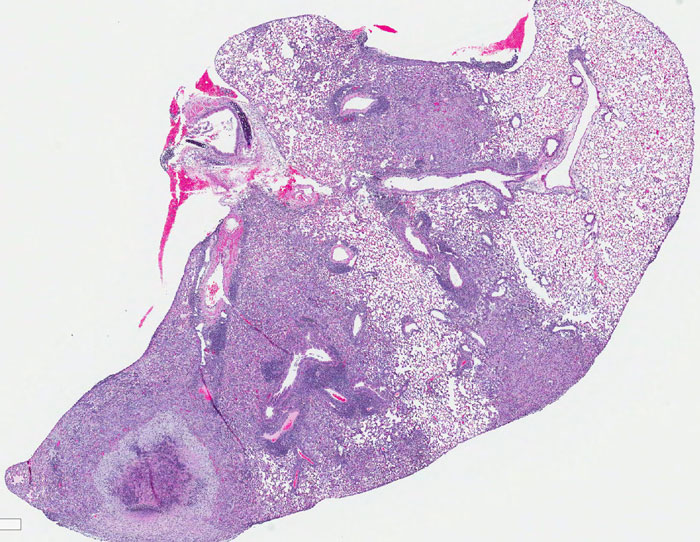
Predicting TB's Course: CIMAR's Gillian Beamer Hopes to Unlock Why the Bacterium Affects Individuals Differently
Beamer plans to identify and test both proteins in blood and lung tissue that accurately determine disease categories and DNA sequences on chromosomes that accurately correlate with these disease outcomes. “Our goal is to generate testable models that can predict the outcome of infection before disease occurs,” Beamer said.
Doctors Are Running Out of Effective Drugs Because of Poor Financial Incentives to Develop Them
Medical researchers have known for decades that the pipeline for new drugs to stave off bacterial infections would one day run dry. That day is now at hand. “The crisis has already arrived. We are in an era now when doctors like me have no effective antibiotics for some of their patients,” says CIMAR Director Dr. Helen Boucher.
Antibiotics Aren’t Profitable Enough for Big Pharma to Make More
Public health experts are calling for new incentives to reward companies for bringing drugs that are effective against resistant strains to market. Achaogen Inc. spent 15 years racing to develop antibiotics against resistant superbugs such as carbapenem-resistant Enterobacteriaceae, or CRE, a strain that can kill up to half the people it attacks. But as a business, it’s a failure. The drug, Zemdri, lacked sales in its first six months on the market == less than $1 million. Achaogen filed for bankruptcy in April.
Medicare Payment Rules Hinder the Fight Against Superbugs
Late last year, a retirement community in Vermont was quarantined after an outbreak of antibiotic-resistant bacteria swept through the facility, sickening 70 seniors. In pediatric oncology wards, children beating cancer are increasingly felled by drug-resistant bacteria and fungal infections. Every week, we hear more stories of infections that have become untreatable due to resistance. Such alarms, once rare, are becoming more commonplace. The time to fix the problem is now, before it’s too late.
Video: CIMAR Professors and Doctors Join Forces to Fight Superbugs
Drug-resistant diseases are hospitalizing and killing people across the world. To fight this crisis, researchers and physicians from Tufts University and Tufts Medical Center are bringing together their unique skillsets under one umbrella: The Tufts Center for Integrated Management of Antimicrobial Resistance.
Archaogen Bankruptcy Raises Worry Over Antibiotic Pipeline
“We’re worried that Achaogen is not alone, and that we will see the fall of other small antibiotic manufacturers,” said Helen Boucher, MD, director of the Tufts Center for Integrated Management of Antimicrobial Resistance and treasurer of the Infectious Diseases Society of America (IDSA). “And we’re worried about the danger this could present for our patients.”
Op-Ed: The Antibiotic Market is Broken and Won't Fix Itself
Over the past year we’ve watched two troubling trends escalate. First, patients increasingly face — and their doctors struggle to treat — infections that do not respond to existing antibiotics. Second, major pharmaceutical companies are backing away from developing new antibiotics.
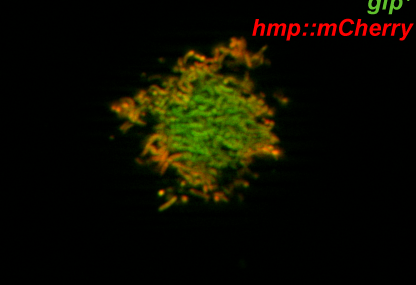
Stopping Cholera in Its Tracks: Testing Bacteriophages as a Way to Halt the Spread of the Deadly Disease
Cholera strikes almost 3 million people each year worldwide. Tufts/CIMAR researchers are developing a treatment to prevent its spread, using viruses to attack the bacterium that causes the disease.
Antimicrobial Resistance Fighters: CIMAR is cracking down on one of the biggest global health concerns
Antimicrobial resistance is a global catastrophe, leading to 700,000 deaths annually around the world. Tufts University and Tufts Medical Center are heeding the call with the new Tufts Center for Integrated Management of Antimicrobial Resistance (CIMAR)…
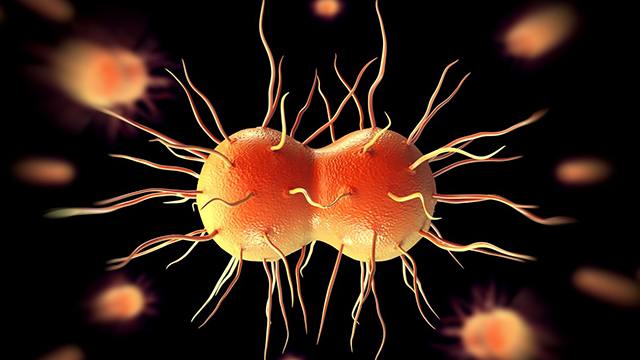
Tufts-Led Study Compares Gender-Specific Expression of Antibiotic Resistance Genes During Active Gonorrhea Infection
The World Health Organization estimates that 78 million people worldwide are infected with gonorrhea each year…
CIMAR Featured in Spotlight on Research and Collaboration
Given an increasingly difficult funding climate, finding the research strengths of the university and focusing resources on those areas is a priority for Tufts. After a year-and-a-half consultative process involving researchers from across the university, five thematic priority areas emerged. …
-
CIMAR Joins the Battle Against AMR with Collaborative and Brainstorming Workshop
The Tufts Center for Integrated Management of Antimicrobial Resistance (CIMAR) hosted its first event last month to introduce the Center to the local scientific community and to offer a platform for investigators and clinicians to showcase their research and promote collaborations.
Tufts Summer Programs Provide Research Opportunities for Undergraduates
Tufts prides itself on being a distinguished research university, providing students with opportunities to apply what they have learned in the classroom to the real world. …
Tufts Researchers Find Link Between Dog-Human Antibiotic Resistance
For many people, pets are family; just as close to them as the humans in their life. However, a new study suggests that closeness can create a concerning health issue making prescribed medicines less effective. …
IDSA announces Tufts Medical Center Among Recipients of Antimicrobial Stewardship Centers of Excellence Designation
The Infectious Diseases Society of America (IDSA) announced today the recipients of its Antimicrobial Stewardship Centers of Excellence (CoE) designation. …