Innovating to Protect Humanity from the Global Threat of Antimicrobial Resistance: Integrating Solutions Across Human and Veterinary Medicine, Stewardship, and Awareness
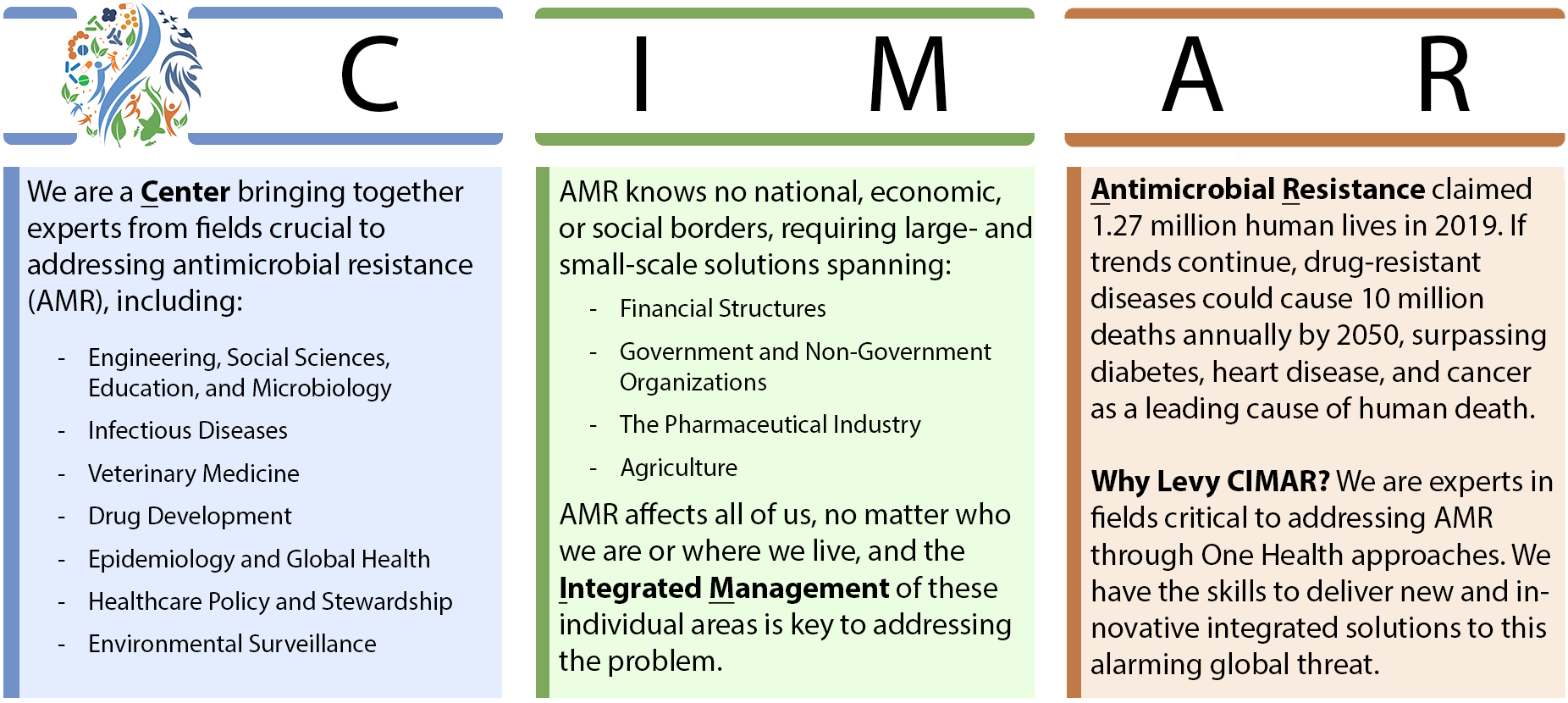
Antimicrobial resistance (AMR) is ranked among the World Health Organization’s top 10 threats to global health. According to the most comprehensive estimate to date on AMR’s global impact, more than 1.27 million people died in 2019 as a direct result of antibiotic-resistant bacterial infections (The Lancet, 2022).
AMR occurs when antimicrobial treatments such as antibiotics, antivirals, and antiparasitics become ineffective against the microorganisms they were created to fight. These microorganism “superbugs” adapt to survive drug treatments, causing infections to persist and spread. With AMR now outpacing the development of new antimicrobial drugs, we risk returning to an era when life-threatening infectious diseases such as tuberculosis and conditions such as pneumonia were a death sentence. If trends continue, drug-resistant diseases could cause 10 million deaths each year by 2050, surpassing diabetes, heart disease, and cancer as a leading cause of human death.
The unfortunate truth about AMR—and what makes it so hard to prevent—is that resistant microorganisms know no borders and can easily spread across the globe and from humans to animals and vice versa. AMR is a complex problem requiring close monitoring and coordination with human and veterinary healthcare, sanitation, education, and government policymakers to prevent its spread. No single sector has the capacity to stop AMR alone. We recognize this and have launched our center to connect and integrate the key players needed to solve this multifaceted problem.
The Stuart B. Levy Center for Integrated Management of Antimicrobial Resistance at Tufts (Levy CIMAR) is a collaborative and cross-disciplinary initiative with a mission to deliver new and innovative solutions to combat AMR. Partnering Tufts Medical Center and Tufts University’s schools of Medicine, Veterinary Medicine, and Arts & Sciences (as well as members from Engineering, Nutrition, and Drug Development) under a single umbrella, the Levy CIMAR is uniquely poised to lead AMR research, drug discovery, patient care, and education. The Levy CIMAR believes that to effectively fight AMR, scientists must take a “One Health” approach to understanding disease transmission and the mechanisms by which we can stop it. One Health prioritizes the relationships among people, animals, the environment, and the foods we all consume as critical avenues by which drug-resistant microorganisms spread from one to another. Our team includes experts in fields critical to addressing AMR through One Health, including microbiology, infectious disease, veterinary medicine, engineering, epidemiology, global health, drug development, and policy.
We believe that together we can preserve the effectiveness of existing antimicrobial drugs and establish a much-needed pipeline to develop new ones.
The Levy CIMAR is organized around four central research areas:
Multidrug Therapies: Using Combination Chemotherapies to Cure Otherwise Untreatable Infections

Combinatorial drug therapies have great potential to both treat infection and diminish the emergence of tolerance and resistance in human and veterinary medicine. A priority research area of the Levy CIMAR is to systematically investigate multidrug regimens for treatment of infectious diseases in the context of learning mechanisms of AMR and developing new antimicrobial strategies. We combine robot-, microdroplet-, and/or biomaterials-based drug screening and testing of drug combinations in animal models. In parallel, we are researching how to adapt the drug approval process for new combinations of previously approved drugs. We aim to fully realize the potential of existing and emerging drugs by developing optimized treatment regimens.
Emerging Treatments: Establishing an Antibiotic Pipeline
Watch this space! We plan to announce some exciting work that we are doing in this area very soon.
Surveillance: Predicting and Preventing Public Health Emergencies Using AMR Data from Our Environment, Communities, and Healthcare Settings

Antimicrobial Surveillance is the ongoing collection, analysis, and interpretation of AMR-related data needed to determine where threats to public health might emerge and what can be done to stop them. We use surveillance strategies and tools from epidemiology, engineering, and the social sciences to monitor sanitation infrastructure, the environment (including water systems and soil), and our communities, including households and healthcare facilities.
Surveillance in the Environment: Preventing Infections at Their Source
Levy CIMAR members use genomic and epidemiological approaches to understand how exposures to food, animals, and the environment can impact human colonization and infection with drug-resistant microorganisms. In tracking and understanding this data, we are striving to develop low-cost and scalable interventions to disrupt transmission.
Levy CIMAR Core Faculty member and Tufts University Assistant Professor of Civil and Environmental Engineering Dr. Amy Pickering (pictured here at right) conducts environmental health research in low-resource settings and has led studies in both urban and rural sites in Kenya, Bangladesh, Mali, India, and Tanzania. Recently, Dr. Pickering and one of her teams found that a novel water treatment device that delivers chlorine automatically via public taps without the need for electricity, reduced child diarrhea (frequently caused by microbes) by 23% compared with controls. Antibiotic usage also went down. This research took place over 14 months in two urban neighborhoods of Bangladesh. (Read more at Science Codex.)
Another group led by Levy CIMAR Core Faculty member Dr. Carol Bascom-Slack (Tufts University’s Center for Translational Science Education) monitors antibiotic-resistant organisms in soil and uses this data to tease out AMR trends and correlations nationally. This educational program, known as the Prevalence of Antibiotic Resistance in the Environment (PARE) project, engages undergraduates in an authentic classroom research experience to shed light on the environmental presence of antimicrobial-resistant microbes. PARE brings together thousands of students at about 125 undergraduate institutions across the country and partner institutes in Botswana and France. They upload data from local soil sites to a shared database, allowing researchers to monitor trends and see where AMR is on the rise. You can learn more about PARE in our Education section or on the program’s official website.
Surveillance in Healthcare: Protecting Patients from Hospital-Acquired Infections
AMR evolves alarmingly fast and requires constant evaluation and reevaluation of resistance patterns to guide medical treatment. Levy CIMAR’s Dr. Shira Doron, an attending physician at Tufts Medical Center and the hospital’s Antimicrobial Steward, relies on surveillance strategies to keep patients on track to maintain their health and get healthier faster. Working with a group from the Worcester Polytechnic Institute in Worcester, Massachusetts, Dr. Doron and team made predictions about which antibiotics would be most effective against which disease-causing microorganisms over the course of up to three years. In their analysis, they used data collected by the Massachusetts Department of Public Health from over 50 acute-care hospitals statewide from 2002 to 2015. The group made their predictions using antibiograms (aggregated reports showing how susceptible specific microorganisms are to different antimicrobials) to determine the best treatment options for patients. Antibiograms are crucial for determining the likelihood of effectiveness of antibiotics even before patient-specific laboratory data is available.
Surveillance is also used as a tool to determine if and where infections are spreading within healthcare settings, where locally acquired pathogens such as Clostridioides difficile can prove deadly to patients, especially those who are already sick with other infections. Each year, nearly half a million people contract C. diff, with most cases occurring in patients on (or recently on) antibiotics. Tufts Medical Center has demonstrated success in lowering C. diff rates in patients. See our section on stewardship for more information on this and other things we are doing to promote responsible antimicrobial use.
Stewardship: Optimizing the Use of Antimicrobials in Humans, Animals, and the Environment

The Tufts Medical Center’s Antimicrobial Stewardship Program provides healthcare workers with guidance for the safe and effective use of antimicrobial agents. We do this by helping to determine whether a patient should be treated with antimicrobial drugs and if so, we promote the selection of the best antimicrobial regimen for that patient, their dosage, and the duration of their therapy. Stewardship programs are important to healthcare facilities of all kinds because they are proven to decrease the development of resistance, improve patient outcomes, and reduce overall healthcare costs.
The Infectious Diseases Society of America (IDSA) has designated Tufts Medical Center as an Antimicrobial Stewardship Center of Excellence (CoE), one of just 25 centers nationally to receive the honor in 2018. We remained an IDSA CoE in 2019 and will receive the honor again in 2020.
Recently, attending physician and Tufts Antimicrobial Stewardship Team member Dr. Gabriela Andujar was named among the first awardees of the Leadership in Epidemiology, Antimicrobial Stewardship, and Public Health (LEAP) Fellowship. This competitive training award is granted to four promising young infectious diseases physicians annually and is funded by the Centers for Disease Control and Prevention. The fellowship aims to foster the next generation of infectious diseases leaders in public health, hospital epidemiology, and antimicrobial stewardship, giving them the hands-on experience they need to lead and collaborate across these disciplines in healthcare. Dr. Andujar is especially interested in antimicrobial stewardship in long-term care settings, antimicrobial resistance, and hospital-acquired infections. The Tufts Medical Center Antimicrobial Stewardship team partners with the Massachusetts Department of Public Health to support long-term care facilities in their efforts to improve upon their stewardship and infection control practices. (You can learn more about Dr. Andujar and her work with the Stewardship Team on our Featured Trainees page.)
Launched in 2003, our Stewardship program performs better than local and national benchmarks in antimicrobial usage and has demonstrated cost savings.
Antimicrobial Stewardship Consulting Services
In addition to our Antimicrobial Stewardship Program, Tufts Medical Center offers consulting services to help other healthcare facilities establish their own programs. Our Tufts Medical Center Experts in Antimicrobial Management (TEAM) program assists organizations with several tasks including but not limited to:
-
- Providing mandated education to care teams
- Applying data analytics to assess current prescribing patterns
- Identifying opportunities for more effective and less costly antibiotic usage
- Regular review of care team performance using established metrics
- Collaborating with healthcare facilities on developing their own policies and protocols
- Consulting with care teams regarding individual cases
According to the Centers for Disease Control and Prevention, 70 percent of the 4.1 million Americans residing in nursing homes receive an antibiotic every year, and up to 75 percent of those antibiotics are prescribed incorrectly—that equates to more than two million inappropriate antibiotic prescriptions annually in nursing home settings alone. Looking at the whole U.S. population, the CDC says that at least one in every three antibiotic prescriptions is unnecessary. Antibiotics are lifesaving drugs and our most powerful tool to fight life-threatening bacterial infections. Overuse and misuse are two of the greatest threats to our limited arsenal of drugs.
Our Antimicrobial Stewardship Team has worked with numerous care facilities to improve antibiotic use and, correspondingly, improve patient outcomes. In collaboration with the Massachusetts Department of Public Health, our team implemented a collaborative quality improvement program to better the management of suspected urinary tract infections in the elderly. About 50 percent of elderly women and 40 percent of elderly men will have urine cultures that test positive for bacteria, however the presence of bacteria does not necessarily indicate an infection or warrant treatment. Our team improved patient outcomes by increasing awareness of current prescription guidelines with a focus on decreasing treatment in patients in the absence of symptoms. As a result, we found a statistically significant reduction in the rate of urine culturing at participating facilities, and UTI diagnosis rates there declined too. We also noted a statistically significant reduction in Clostridioides difficile rates.
Another facility that has benefited from our team’s consulting is the New England Sinai Hospital in Stoughton, Massachusetts, a long-term acute-care hospital for patients who are chronically and critically ill. There, we developed 885 individualized recommendations for the treatment of 734 patients, resulting in fewer antibiotics prescribed and markedly decreased rates of C. diff infection.
Education: Raising AMR Awareness Through Academics and Community Outreach

Tufts educators are leading the way in AMR curriculum development and implementation for trainees starting at the high school level through undergraduate, graduate, and postgraduate education. We offer educational programs on AMR with an emphasis on cross-campus efforts, giving our trainees first-hand exposure to real-life research, medicine, and more. Our programs provide a connection between discovery and patient care at the individual and population level and ensure a presence of a robust and sustainable workforce with the knowledge and competencies needed to combat AMR and promote stewardship.
Tufts Mini-Med School: Experience What it Takes to be a Healthcare Professional
In July 2020, Levy CIMAR Core Faculty and colleagues launched “Tufts Mini-Med School,” an intensive summer program for driven high schoolers interested in medical school (or in other health professions). Through lectures and medical case studies coupled with hands-on training, students got a taste of what it takes to study medical sciences. The program was held virtually this year due to the COVID-19 pandemic, but was still a huge success with 700+ applicants worldwide applying for just 125 slots.
Students learned how infectious diseases are diagnosed, the importance of appropriate treatment, and the challenges doctors face today in combating multi-drug resistance. They also learned about the cutting-edge solutions to these challenges that Levy CIMAR and other researchers are developing.
With the belief that the future of medicine and medical training is a One Health approach, Tufts Mini-Med School is uniquely interdisciplinary and is distinctive in its ability to draw on the stunning array of schools (beyond the School of Medicine) dedicated to the health science and medicine at Tufts University, including: the School of Dental Medicine, the Cummings School of Veterinary Medicine, the Friedman School of Nutrition Science & Policy, and the Graduate School of Biomedical Sciences. Please click here to learn about Tufts Mini-Med School and how things went this summer.
PARE Program: Join a Nationwide Network of Citizen Scientists Surveilling AMR in the Environment
Several Levy CIMAR members interested in surveillance methods and data gathering are involved with another program called PARE, the Prevalence of Antibiotic-Resistance in the Environment project. PARE is a course-based and citizen-science driven research project with goals of large-scale monitoring of antibiotic-resistant organisms in the environment. PARE provides a low-hurdle pathway for instructors to begin implementing research in their classrooms. The project brings together thousands of students at about 125 undergraduate institutions across the country and partner institutes in Botswana and France. They upload data from local soil sites to a shared database, allowing researchers to monitor trends and see where AMR is on the rise. You can learn more about PARE on the program’s official website.
The slideshow at the bottom of this section includes photos from PARE collaborators in the United States and abroad. The first set is from a PARE partner in Botswana, while the second depicts the work of the College Bound Explorers program at Pine Manor College.
Levy CIMAR Outreach Efforts: Engaging Our Communities to Join the Fight Against AMR
The Levy CIMAR hosts scientific workshops and symposia in an effort to support collaboration and to further research. We also host outreach events for other members of the community who are not professional scientists, but who have an interest in infectious diseases and AMR.
We held our first such event in 2019 for 33 students from Boston-area Brockton High School. The students presented posters depicting original experiments and data on antimicrobial resistance to a wide audience of Tufts University and Tufts Medical Center graduate students, postdoctoral fellows, faculty, and clinicians. The students also got to meet and learn from Levy CIMAR’s experts in AMR through presentations of case studies, one-on-one interactions, and a panel discussion.
The Levy CIMAR also participated in the first Tufts@Kendall event, which connected Tufts researchers and members of the biomedical industry.Hosted by Tufts Corporate and Foundation Relations and MassBio, the event focused on the tagline, “Breaking the Chain of Infection: Innovations in the Prevention and Treatment of Infectious Disease.” More than 80 members of the biomedical community, including representatives from 20 different companies, came together to learn and discuss the latest advances in infectious disease and antimicrobial resistance at the Levy CIMAR.
We have several outreach events coming in the future. To stay up-to-date with what the Levy CIMAR is doing, please visit our News and Events pages.
Featured Trainees
If you’d like to read more about how the Levy CIMAR is educating trainees in our own labs and clinics, please visit our Featured Trainees page. Featured Trainees are students, postdoctoral fellows, practicing physicians and faculty, and others who work under the tutelage of Levy CIMAR Core Faculty members and who stand out for their efforts in the fight against antimicrobial resistance. Trainees might be graduate students, antimicrobial stewards, educators, scientific researchers, medical doctors, veterinarians, pharmacists, or a combination of any of these and other professions.
Our Values: Diversity, Equity, and Inclusion
The Levy CIMAR is committed to a culture of diversity, equity, and inclusion both within our organization and for all people who are impacted by our work. We strive for health equity for people from all backgrounds and identities, and we actively support societal and institutional structures that promote justice and equality. We are also committed to being a safe, respectful, and inclusive environment for our trainees, staff, faculty, affiliates, and partners. One Health acknowledges the interconnectedness of all humans, along with animals and our environments. Antimicrobial resistance impacts us all.

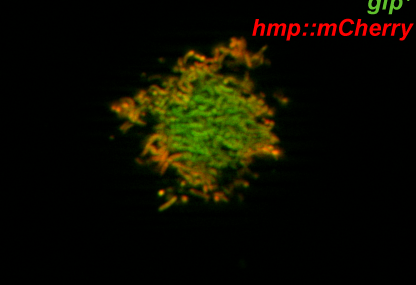
(The image above depicts members from the Bree Aldridge Lab @ Tufts.)