Levy CIMAR Promotes One Health, Collaboration Through “Fighting AMR Together” Workshop

Dr. Deborah Hung of the Broad Institute of MIT & Harvard gears up for her keynote address, “Antibiotic Discovery and Development: The Challenge of Bench to Bedside.” (Photo Credit: Levy CIMAR Director Dr. Helen Boucher)
Nov. 19, 2020
Rima Mycynek
The Levy CIMAR hosted our second annual collaborative workshop titled “Fighting AMR Together” earlier this month. The event offered a platform for investigators and clinicians to showcase their research and promoted opportunities for partnership both within and outside of the Tufts network.
The Levy CIMAR addresses antimicrobial resistance (AMR) through multidisciplinary approaches around themes including combination drug therapies, surveillance and stewardship from a One Health perspective, as well as education and community outreach. The Center has received funding from both Tufts Medical Center and the Tufts University Office of the Vice Provost for Research (OVPR) Research and Scholarship Strategic Plan (RSSP) to support platform development, seminar series, symposia, workshops, seed grants, and industry collaborations. Now in the start of our third year, we are proud to report that we have made strides in all of these areas.
The two-day workshop, held Nov. 5-6, 2020, began with welcoming remarks from Levy CIMAR Director Helen Boucher, MD, Senior Leadership member, John Leong, MD/PhD, and Executive Director Brian Noonan, PhD, on the Center’s achievements so far and our plans for the near future. Under Dr. Noonan, the Levy CIMAR is working to become self-sustaining. We are in the planning stages of several projects including educational programs for all academic levels from high school to professional continuing education, increased industry collaboration, and building core laboratory facilities.
The workshop featured talks from four of the Levy CIMAR’s seed funding awardees on their pilot projects, ten research talks from Levy CIMAR investigators and colleagues at Paratek Pharmaceuticals, Northeastern University, and Boston College, and a keynote address from Dr. Deborah Hung of the Broad Institute of MIT & Harvard.
Fighting AMR Together
In her talk, “Antibiotic Discovery and Development: The Challenge of Bench to Bedside,” Dr. Hung discussed the challenges scientists face when trying to get new antimicrobials to market and into the hands of medical professionals. After Alexander Fleming discovered the antibiotic penicillin in 1928, many healthcare professionals believed infectious diseases would become significantly easier to treat. And they did. But as antibiotics have been overprescribed and misused, bacterial pathogens have evolved new defenses, becoming antimicrobial-resistant “superbugs” that render previously effective drugs useless. AMR is ranked among the World Health Organization’s top 10 threats to global health, with 700,000 people dying annually from drug-resistant infectious diseases. If trends continue, drug-resistant diseases could cause 10 million deaths each year by 2050, surpassing diabetes, heart disease, and cancer as a leading cause of human death.
With the rate of resistance is outpacing our ability to get new antibiotics to market, Dr. Hung has had to tell patients with highly resistant infections that there would be no more effective treatments for them, essentially giving them a death sentence. Dr. Hung and other experts agree: The next pandemic could be bacterial, and before that happens, we must repair what has become a fundamentally broken system.
“We need a game changer,” said Dr. Hung. “We have to think about how we address the science. We can’t only focus on Alexander Fleming-style antibiotics.”
The unfortunate truth about AMR—and what makes it so hard to prevent—is that resistant microorganisms know no borders and can easily spread across the globe and from humans to animals and vice versa. AMR is a complex problem requiring close monitoring and coordination with human and veterinary healthcare, sanitation, education, and government policymakers to prevent its spread. No single sector has the capacity to stop AMR alone.
Fortunately, scientists, clinicians, policymakers, and others worldwide are launching efforts to combat these problems, and the Levy CIMAR believes that our faculty possess the myriad unique skillsets needed to help lead this fight. Our roster includes 29 core faculty and five senior leaders from Tufts Medical Center and Tufts University’s schools of Medicine, Veterinary Medicine, Nutrition Science & Policy, Arts & Sciences, and Engineering as well as the Center for Science Education and the Center for the Study of Drug Development.
Levy CIMAR Seed-Funded Pilot Projects
The Levy CIMAR has funded five ongoing pilot research projects so far from Core Faculty members Drs. Michael Jordan, Bree Aldridge and Roberto Viau, Amanda Martinot, and Amy Pickering. The projects each focus on new and innovative science addressing AMR. Our investigators discussed four of these projects:
“Multi-Drug Therapy for Drug Resistant Bacterial Infections” (Aldridge, Viau): As AMR increases, clinicians face more patients with multi-drug resistant infections or biofilms. Laboratory assays to test multi-drug interactions are rarely used in medical microbiology labs, and so the combination therapies are often chosen without strain-specific empiric data. Levy CIMAR investigators aim to compare clinical outcomes with DiaMOND measurement in clinical isolates to define a path for combination drug measurement in research and medical microbiology laboratories to improve treatment outcomes in patients.
“Point of Care Urine Tenofovir Testing as a Predictor of HIV Viral Load Suppression in Lesotho” (Jordan): Current methods for determining patient adherence to antiretroviral therapies are flawed due to self-reporting bias or high cost. Measuring drug levels in combination with adherence counseling leads to improved adherence and improved patient outcomes. Dr. Jordan and colleagues believe that measuring tenofovir in urine provides an inexpensive, effective, and reliable method of monitoring adherence and may lead to refinements in global HIV viral load and genotyping algorithms to maximize population-level viral load suppression.
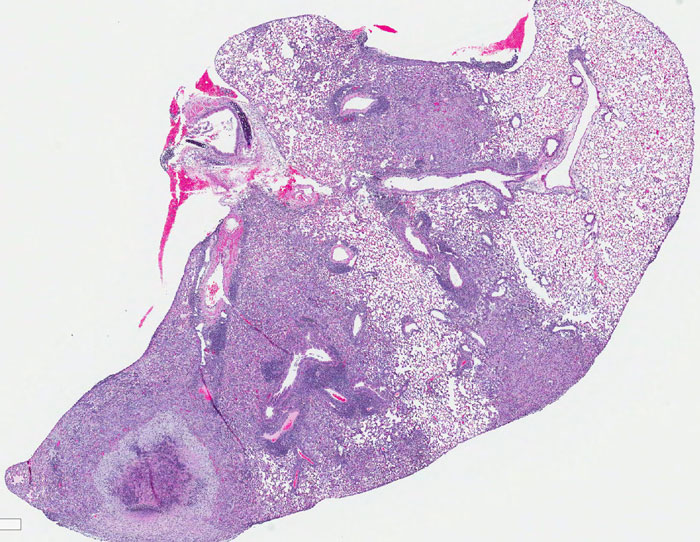
“Combination Immunotherapy to Treat Multi-Drug Resistant Tuberculosis” (Martinot): Tuberculosis is complex disease characterized by disease latency and reactivation and requiring long-term antibiotic treatment. Unfortunately, tuberculosis can easily become resistant to therapies, so combinations of drugs are required for effective treatment. Dr. Martinot and team are looking into the possibility of a post-exposure vaccination as an effective intervention for drug resistant TB.
“Tracking Antibiotic Resistant Bacteria Between Humans, Animals and the Environment with Long-Read Metagenomics” (Pickering): Antibiotic resistant infections are a critical threat to public health, especially in low-and middle-income countries where limited access to safe drinking water and adequate sanitation as well as close proximity to animals exacerbates the spread. To better prevent antimicrobial resistant infections, a stronger understanding of transmission of AMR between humans and animals is needed. In addition, surrounding humans and animals lie environmental transmission pathways, which can serve as reservoirs for AMR. In this Levy CIMAR funded project, researchers are investigating the sharing of antibiotic resistance genes and antibiotic-resistant bacteria between humans, poultry and the environment (soil) in poultry-owning households in Nairobi, Kenya. The goal of this work is to determine which pathways are important in transmission of AMR in order to inform the design of adequate interventions to block the spread.
The Four Focus Areas of the Levy CIMAR
Although the more than 20 researchers who spoke at CIMAR’s workshop presented on numerous fascinating areas of AMR-related science, medicine, and policy, the overarching themes can be categorized into the Levy CIMAR’s four main areas of focus: education and promoting community awareness, multidrug therapies, environmental surveillance, stewardship in human and animal medicine. Here are the highlights:
Education: Raising AMR Awareness Through Academics and Community Outreach
The educational arm of the Levy CIMAR provides free resources to educators, students/trainees, and others interested in materials that help explain and distill concepts pertaining to antimicrobial resistance. They also engage in programs like the wildly successful Tufts Mini-Med School held this past July, which despite having to go from in-person to online due to the COVID-19 pandemic, boasted over 700 applicants for just 125 slots. Tufts Mini Med School will be back in 2021 and soon, the Levy CIMAR develop more curricula for all education levels beginning with high school.
Core Faculty members Carol Bascom-Slack, PhD, Berri Jacque, PhD (Center for Science Education), and Dr. Maya Nadimpalli, PhD (School of Engineering) presented, “Unifying our Message through a One Health Approach: Levy CIMAR’s Education Initiatives.” In science and medicine, One Health prioritizes the relationships among people, animals, the environment, and the foods we all consume as critical avenues by which drug-resistant microorganisms spread from one to another. In the context of our educational approaches, One Health similarly prioritizes scholarship (answering questions no one yet has the answers to), education (delivering training and tools), and measuring impact (designing interventions that change behavior).
Tracy E. Schmidt, PhD (Director, Corporate and Foundation Relations, Health Sciences) and Susan Lewis, PhD (Associate Director, Research Development, Office of the Vice Provost for Research) offered several resources for funding support for graduate students and post-doctorates. (You can find these on our Educational Resources page.)
Multidrug Therapies: Using Combination Chemotherapies to Cure Otherwise Untreatable Infections
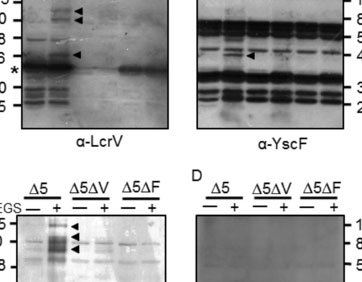
Levy CIMAR Associate Director Bree Aldridge presented on DiaMOND (Diagonal Measurement of n-way Drug Interactions), a method used by the Aldridge Lab to systemically study pairwise and high-order drug combinations to develop shorter, more efficient treatment regimens for bacterial infections. Combinations of three or more drugs are used to treat many diseases, including tuberculosis, and it is important to understand how synergistic or antagonistic drug interactions affect the efficacy of combination therapies. Previously, scientists’ understanding of high-order drug interactions was limited because of the lack of both efficient measurement methods and theoretical framework for analysis and interpretation. DiaMOND provides an efficient alternative to checkerboard assays, which are commonly used to measure drug interactions. (You can learn more about DiaMOND here.)
Levy CIMAR investigator Joan Mecsas, PhD, and her lab, including workshop presenter and MD/PhD student Yoelkys Moralis, are working with the Aldridge Lab to optimize the DiaMOND platform for multi-drug resistant Klebsiella infections. They are particularly interested in how drug interactions change in different conditions that mimic infection site environments, and have discovered that conditions that mimic lung and bladder infections produce different drug interactions than those found in more traditional media. The Mecsas Lab have also found that results in drug-sensitive strains do not predict how drugs will interact in a drug-resistant strain.
Patients suffering from tuberculosis, caused by Mycobacterium tuberculosis (Mtb) face a long and arduous course of treatment even in the best of circumstances. On top of this, multi-drug resistant Mtb is a growing problem worldwide. The development of new antitubercular drugs could help in the development of new and more effective TB treatment regimens. Under the guidance of Dr. Aldridge, Trever Smith, PhD, and colleagues have developed MorphEUS (Morphological Evaluation and Understanding of Stress) a new imaging and analysis pipeline to rapidly identify how drugs kill Mtb.
Another useful technology for rapid and accurate diagnostics is called G-FET (Graphene Field Effect Transistors). Point-of-care diagnostics that are able to reduce and/or prevent unneeded antibiotic prescriptions require highly specific probes with sensitive and accurate transducers that can be miniaturized and multiplexed, and that are easy to operate and cheap. Juance Ortiz-Marquez, PhD, a postdoctoral scholar in the Dr. Tim van Opijnen Lab at Boston College, presented on a number of advances in the use of G-FET including the first use of peptide probes to electrically detect antibiotic resistant bacteria in a highly specific manner.
Of course, in order to understand what therapies might work best, it’s also important to examine how drug resistance emerges in bacteria and seek out vulnerable targets for attack within these bacteria.
Edward Geisinger, MD, PhD, of Northteastern University says that the antibiotic-resistant pathogen Acinetobacter baumannii has evolved unique strategies to build its cell envelope and divide. Dr. Geisinger and team have identified mutations throughout the A. baumannii genome that alter antibiotic susceptibility and used this information to discover the function of uncharacterized proteins involved in envelope biosynthesis and division. He says that antibiotic susceptibility signatures identify targets for attack in the A. baumannii cell envelope.
Levy CIMAR Director Ralph Isberg and his lab are also looking for an Achilles’ heel that will make A. baumannii more vulnerable to therapies. Presenter Efrat Hamami, a PhD student in the Isberg lab, and colleagues are investigating high-level fluoroquinolone resistance in strains of the bacterium, particularly those that demonstrate high levels of resistance due to drug egress pump overproduction. They are working to identify proteins that may protect against stressors that result from pump overproduction, as these proteins may serve as candidate targets to re-sensitize these pathogens to fluoroquinolones or otherwise eliminate such highly resistant strains from a population.
Stewardship: Optimizing the Use of Antimicrobials and Increasing Access to Novel Drugs
Tufts Veterinarians Annie Wayne and Claire Fellman have a One Health partnership with Tufts Medical Center’s chief epidemiologist Shira Doron and pharmacist Kira Beaulac to apply antimicrobial stewardship to small animal veterinary clinical settings. In their talk, “Stewardship in Small Animal Veterinary Medicine,” Drs. Wayne and Fellman discussed their aim to create automated data systems to describe and track antimicrobial use in dogs and cats to target and measure the effect of stewardship interventions.
Evan Loh, MD, CEO of Paratek Pharmaceuticals, noted that there are several barriers in the way of promoting stewardship, including limited access to new and novel drugs. It can cost $1.5 billion to bring a new antibiotic to market, resulting in a net loss in the tens of millions of dollars for most pharmaceutical companies producing successful drugs. And with that in mind, it is estimated that only about one in 15 antibiotics in the preclinical stages will make it to market. Many biotech companies have thus exited the business, are struggling on the brink of financial collapse, or are facing bankruptcy. Dr. Loh says if we are going to ensure that we have the antimicrobials we need to continue to fight infections that are resistant to commonplace drugs the marketplace needs to recognize the value of innovation and that starts with government policy reforms, some of which are currently in the works (for example the DISARM and PASTEUR Acts).
Prescribing the right drugs can make all the difference for patient outcomes. In her research talk, Levy CIMAR’s Cheleste Thorpe, MD, of Tufts Medical Center, described how antibiotic treatment choices for Clostridioides difficile infection differentially affects microbiota and bile acid composition in the human gut over time. Compared to vancomycin (a standard of care), the investigational narrow-spectrum agent preserved secondary bile acids, which may explain the higher sustained clinical response observed in subjects who received it.
Surveillance: Predicting and Preventing Public Health Emergencies Using AMR Data from Our Environment, Communities, and Healthcare Settings
Levy CIMAR investigator, Maya Nadimpalli, PhD, of the Tufts University School of Engineering, says that there is growing interest in the role that improved water, sanitation, and hygiene (WASH) interventions could play in curbing the spread of antibiotic resistance, particularly in low-resource settings. Dr. Nadimpalli presented data from an ongoing study that is investigating the impact of water chlorination on young children’s gut microbiomes and resistomes in urban Bangladesh. Samples were obtained from a cluster-randomized water chlorination intervention trial that significantly reduced children’s diarrhea and recent antibiotic use, leading Dr. Nadimpalli and colleagues to hypothesize that water chlorination could have reduced children’s gut colonization with antibiotic resistance genes, as well. Although water chlorination appeared to have significantly altered children’s gut microbiomes, the relative abundance of antibiotic resistance genes in the gut was unchanged. It is possible that children in this study were exposed to antibiotic resistance genes via alternate routes besides water (e.g. food), that 6 months of exposure to chlorinated water was not sufficiently long enough to reduce the abundance of resistance genes in the gut, and/or that multiple WASH interventions are needed to truly curb resistance in this setting.
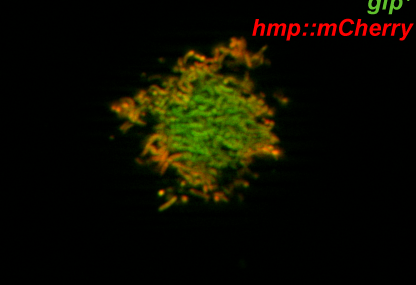
In her talk, “Sex and the Superbug,” Caroline Genco, PhD & Vice Provost for Research, Tufts University School of Medicine discussed how she and colleagues are tracking AMR Neisseria gonorrhoeae infections and disease transmission between infected men and asymptomatic women. Using whole RNA-seq, they aim to understand gender-specific gene expression that may explain the relative prevalence of asymptomatic gonorrhea infections in women as compared to men.
A Look to the Future
In the era of COVID-19, we are more concerned than ever about the rise in infections caused by resistant superbugs. Antibiotics are widely prescribed to patients even without signs of bacterial co-infections, which we know will have the downstream effect of diminishing antibiotic supplies and increased rates of AMR. Partnering Tufts Medical Center and Tufts University’s schools of Medicine, Veterinary Medicine, and Arts & Sciences, as well as members from Engineering, Nutrition, and Drug Development, under a single umbrella, we feel the Levy CIMAR is uniquely poised to lead AMR research, drug discovery, patient care, and education.